- Brokerage New Construction How to Buy How to Sell
- Yacht Fleet Yacht Catalog Charter Marketing Destination Guides
- Financial Services Payroll & Accounting Payroll Service Process Logistical Support Admin Services Crew Admin
- Job Descriptions Crew FAQ
- About Sitemap

- Yacht Department Directory
- Engineering Department

Electronics Engineer (ETO)
About the electronics engineer (eto).
The ETO is a vital part of the AV/IT experience on board a mega yacht. This engineering role is specifically focused on the audio-visual systems on board including the TV’s, sound systems, movie projectors and making sure every guest can watch a movie on the iPad if requested. Strong computer and networking skills are a must. The successful candidate has an electronics background, is a skilled troubleshooter, has the personality to interact and work with guests directly and will enjoy the challenge of complex AV/IT systems aboard superyachts. The ETO may also be asked to help with other engineering duties as needed and has at least two years in similar roles.

Job Responsibilities
- Day-to-day maintenance of all electronic, computer, audio/visual and communications equipment and ensures its efficient operation
- Ensuring that all planned maintenance work takes place on these systems and co-ordinates operations with shore-side technicians
- Increasing knowledge of all systems on board
- Continued education and licensing
Required Skills
- Prior experience working with IT/AV equipment
- Team player, able to assist with some deck duties; line handling, water sports
- Flexible and adaptable
Salary Modifiers
- Engineering or electronics degree
- Brand/type specific certification (i.e. Crestron, Apple, networking)
- Tender driving certification
Position Statistics
Career path, chief engineer unlimited, chief y1 (<3000gt < 9000kw), chief y2 (<3000gt < 3000kw), chief y3 (<500gt < 3000kw), chief y4 (<200gt < 1500kw), 2nd unlimited, 2nd (<3000gt <6000kw), 2nd (<3000gt <3000kw), 2nd (<500gt <3000kw), oow engineer (meol), oow engineer (aec), junior engineer (unlicensed).
Essential Guides
Ocean Mapping
New to Yachting
Electro Technical Officer jobs
Your new adventure awaits.

Explore more yacht roles
Other essential guides.

Mandatory certificates

What you need to know about B1/B2 visa

Download yacht crew CV templates

How to write a memorable yachting CV

How to prepare for a yacht interview?

What are the two main yachting seasons?

Big yacht crew hubs you should know about

Is yachting the right choice for me?

Yacht crew salary guide
ETO Officer works with electrical systems and high voltage to ensure safe performance of the yacht’s electrical systems.
ETO stands for “Electro–Technical Officer”. This position encompasses any task onboard that works with electrical systems on Heating Ventilation Air conditioning (HVAC), High Voltage (HV) and sometimes Diesel Electric systems to ensure their safe performance.
Yachts over 100m | 330ft in length generally have both a dedicated ETO and a dedicated AV/IT Officer due to the scale of technology and systems on board.
What does a yacht ETO do? | Yacht ETO Job Description
The ETOs take a specialist role within the Engineering Department and are responsible for maintaining a wide range of complex electric systems onboard a yacht.
The responsibilities of an ETO include:
Ensuring proper work and maintenance of all electrical equipment on board
Working of electrical parts like engine rooms, radio communications, and electronic navigation needs
Look into basic electric needs like refrigeration, bridge systems and control rooms
In charge of maintenance of all switchboards including the main switchboard and emergency switchboard
Responsible for all the batteries that are connected to machinery onboard
Maintenance of the HVAC system
Maintenance of emergency systems including emergency switches, fire alarms and detectors
Maintenance of the yacht’s electrical components like navigational lights, battery backups and electrically operated propelling machinery
Arranging and managing external contractor visits when needed
Soft and hard skills required to be an ETO
An ETO should be a self-motivated person, capable of working unsupervised and show superior knowledge in electrical systems. They are the go-to person for any electrical issues so they must have knowledge and confidence in resolving a myriad of problems that may arise.
The skills of an ETO include:
Experience in electrical power supply and distribution systems
A working understanding of risk assessment procedures, safe systems of work and planned maintenance requirements
Independent decision-making capacity
Ability to work under pressure
Task prioritization and organization
Strong communication and interpersonal skills
Mandatory certificates needed to work on board a yacht
All crew members regardless of position and seniority need to have a valid STCW Basic Safety Training certificate, along with a recognised Seafarers medical certificate, the most popular being the ENG1 which is issued by an MCA (Maritime and Coastguard Agency) professional medic.
Without these two certificates, it is not possible for crew to work on board a yacht and a Recruiter will not be able to assist you in finding work onboard a yacht. For more information about mandatory certificates please visit our Mandatory Certificates Guide .
Are you ready to secure an ETO position on board a yacht?
Become a member of YPI CREW and connect with our recruiters so they can guide you through your job search.
Each of our recruiters is specialised in crew placement for a particular department and they will do their best to get you an interview on board a yacht. They will also advise you on how to best present your experience and skills and prepare for a yacht job interview.
YPI CREW TEAM
Ypi crew recruiters in charge of yacht eto recruitment.

Jacqui Young
Head of Engineering Department

Marjorie Baillet
Engineering Recruitment Specialist

Let’s get started. Call us on +33 (0)4 92 90 46 10 or email us.
Our mission, vision and values, mlc 2006 compliance, essential guides, yacht crew positions.
Chief Officer
Second Officer
Third Officer
Chief Engineer
Interior Crew
Head of Service
Head of Housekeeping
Specialist Positions
Spa Manager
Spa Therapist
Personal Trainer & Yoga Instructor
Hairdresser
Mandatory Certificates
B1/b2 visa information, how to write a memorable cv, how to prepare for an interview, yachting seasons, yacht crew salary guide, is yachting the right choice for me, cv templates, ocean mapping, new to yachting.
+33 (0)4 92 90 46 10
Electrotechnical Officer Jobs
Welcome to the viking crew maritime job search portal for eto.
The electro-technical officer is in charge of the ship’s communications systems, electronic systems, and computer systems.
As an ETO, you could work on a range of vessels from cargo ships and large vessels to passenger cruises and superyachts.
Below you will see all of the latest jobs as an ETO in the maritime industry available via Viking Crew – The leading cruise, commercial and superyacht maritime crew services provider.
- 2nd Electrician
- 2nd Engineer
- 3rd Officer
- 4th Officer
- Assistant Shop Manager
- Assistant Sommelier
- AV/IT Officer
- Chef De Partie
- Chef De Partie - Pastry
- Chief Engineer
- Chief Officer
- Chief Purser
- Chief Steward/ess
- Crew Purser
- Deck / Stew
- Deckhand/Carpenter
- Deckhand/Medic
- Demi Chef de Partie
- Destination Manager
- Destinations Services Advisor
- Entertainment Manager
- Executive Chef
- Executive Sous Chef
- Food and Beverage Manager
- Future Cruise
- Hair Stylist
- Head Mixologist
- Head of Service
- Hotel Department
- Hotel Director
- Hotel Engineer
- Hotel Manager
- Housekeeping Steward/ess
- Laundry Steward/ess
- Lead Service Stewardess
- Lifestyle Concierge
- Nail Technician
- Placement Consultant
- Service Steward/ess
- Service Utility
- Shop Assistant
- Shop Manager
- Shop Specialist
- Shore Ex Assistant
- Shore Ex Manager
- Shorebased Position
- Sole Engineer
- Spa Manager
- Spa Therapist
- Staff Chief Engineer
- Stew/Masseuse
- Technical Communications Officer
- Wellbeing Coach
Specialist Skills
- Access Control
- Accountancy Software (Quickbooks)
- Accountancy Software (Sage)
- Accountancy Software (Zero)
- Accounting & Budgeting
- Acrylic Nails
- Acupuncture
- Administration
- Air Conditioning
- Allergies Cuisine
- American Cuisine
- American Service
- Aromatherapy
- Atkins Cuisine
- Azerbaijani
- Azimut Drive (360 Rotation)
- Bashkort (Bashkir)
- Beach Set Ups
- Boat Building
- Bow Thruster
- Bridge Publications
- Bridge Systems
- Brow Treatment
- Bss Sound Web
- Buffet Service
- Caribbean Cuisine
- Carpet Care
- casino dealer
- Chart Corrections
- Child Care (Nannying)
- Chinese Cuisine
- Chocolatier
- Cigar knowledge
- Cleaning & Detailing
- Cocktail Knowledge
- Cocktail Making
- Coffee Making
- Communication
- Computer Skills
- Crane Operation
- Customer Relationship Management Crm Software
- Data Administration
- Data Analysis & Storage
- Deep Tissue
- Diesel Electric
- Diesel Engines
- Dining Management Software
- Discjockey/Dj
- Drone Operations
- Eastern European Cuisine
- Electro Hydraulic Controls
- Engineering
- Entertainment Systems
- Event Management
- Eyelash Treatment
- Fibreglass Repairs
- Filing & Fairing
- Firewall/Security
- Fleet Management Software
- Fly Boarding
- Frb Driving
- French Cuisine
- French Service
- Fruit Carving
- Fuel Cell Systems
- Fusion Cuisine
- Galley Assistance
- Gas Fuel Or Tri Fuel
- Gas Turbine
- General Repairs & Maintenance
- Generators & Alternators
- German Cuisine
- Greek Cuisine
- Guest Reservations.
- Hair Extensions
- Hair Styling
- Hairdresser
- Haitian Creole
- Hammam Ritual
- Hawaiian Creole
- Healthy (Low Fat) Cuisine
- High Voltage
- Hospitality
- Hydraulic Systems
- Ice Carving
- Ice Navigation
- ICU Experience
- IDEA knowledge
- Indian Cuisine
- Indian Head
- Indonesian (Bahasa Indonesia)
- Inflatables
- Installation/Configuration
- Interval Training
- Inuit/Inupiaq
- Irish Gaelic
- Ism/Isps Procedures
- It/Customer Support
- Italian Cuisine
- Itinerary Planning
- Japanese Cuisine
- Kaleidescape
- Kite Surfing
- Knots Knowledge
- Kosher Cuisine
- Laundry & Housekeeping
- Lighting Systems
- Line Handling
- make up artist
- Malay (Bahasa Melayu)
- Mandarin (Chinese)
- Martial Arts
- Massage Techniques
- Mediterranean
- Mexican Cuisine
- Microsoft Excel
- Microsoft Outlook
- Microsoft Powerpoint
- Microsoft Word
- Mid Eastern Cuisine
- Molecular Cuisine
- Mooring Operations
- Nail Construction
- Nail Painting
- Napkin Folding
- Nas Systems
- Network Support
- New Build Experience
- Nouvelle Cuisine
- Nutritian & Diet Plans
- Outboard Engines
- Pacific Rim Cuisine
- Paddle Boarding
- Personal Trainer
- Pescaterian
- Photography
- Planned Maintenance Systems
- Plated Service
- Polar Waters
- Provisioning
- Radio Systems
- Refit Experience
- Reflexology
- Refrigeration
- Russian Service
- Sail Repairs
- Sandblasting
- Satelite Communications Systems
- Search Engine Optimisation (Seo)
- Shellac Nails
- Shipboard Property Management Software
- shipyard period
- Silver Service
- Simulator Instructor
- Single Screw
- Single Screw (With Kort Nozzle)
- Software Devlopment & Engineering
- Spanish Cuisine
- Spear Fishing
- Stand Up Jet Ski
- Steam Turbine
- Steering Gear
- Table Service & Settings
- Tea Service
- Teak Maintenance
- Teak Repair
- Technical Drawings
- Television/Tv
- Tender Driving
- Tender Operations
- Touch Panels
- Troubleshooting
- Twin Screw (With Kort Nozzle)
- Underwater Videography
- Vegetarian Cuisine
- Video On Demand
- Videography
- Visa Knowledge
- Wake Boarding
- Wake Surfing
- Wardrobe Management
- Watchkeeping
- Water Jet Propulsion (Inc Jet Skis)
- Water Makers
- Water Treatment
- Waterskiing
- Watersports
- Web Devlopment
- Windlass & Winch Systems
- Window Treatment
- Wine Knowledge
- Wraps Srubs
- Health & Beauty
- East Mediterranean
- Indian Ocean
- Middle East
- Netherlands
- Northern Europe
- South of France
Temporary Captain 35m Private motor yacht
Viking Crew are looking for a Temporary Captain to join a 35m private Motor yacht in Doha. Candidate must have experience as a captain on similar size vessel Master 500GT COC ECDIS<...
Share This Job
Chief officer required for 100m+ private yacht.
We are looking for a Chief Officer for a 100m+ private yacht Position to start in July Candidates must have: Master Unlimited STCW Basic Training ENG1 HLO Cruise and Y...
Stew/Masseuse needed for 70M private yacht in the USA
Viking Crew is looking for a Stew / Masseuse for a 70M+ private yacht, currently in Florida. Candidates should be good all rounders - and will be assisting in service when guests on. ...
Experienced Chief Stewardess 35m private motor yacht
Viking Crew are looking for a Chief Stewardess to join a 35m private motor yacht . Based in the middle East Shore side accommodation and transport also provided Start date: ASAP ...
Laundry Stewardess needed for 80M+ private yacht
Viking Crew is looking for a Laundry Stew for an 80M private/charter yacht. Candidates must be proficient in the laundry, with a good understanding of different detergents and laundering equi...
We are searching for an Entertainment & Engagement Manager to join a luxury cruise line
An Entertainment & Engagement Manager is required for a luxury cruise company. The Entertainment Manager is responsible for the management and day-to-day running of all aspects of onboa...
Spa Manager for 80 M private yacht
Spa Manager needed for 80 M private/charter motoryacht. Candidates need to have previous experience onboard yacht with proven longevity. When the Spa Manager is not busy in the Spa with trea...
Captain needed for 55ft dayboat in South of France
Viking Crew is looking for a Captain for a 55ft dayboat, located in the South of France. seasonal position - accommodation provided ashore Local cruising in the St Tropez area - a ...
Sole Engineer 35M motor yacht
Viking Crew are looking for a Sole Engineer to join a 35M motor yacht in the South Pacific Seasonal position Must have STCW ENG1 Start date ASAP 30th May- End of September. We are looking for a Port Vessel Unit Engineer (PVU) for a UK port. Contract: Permanent Shift Pattern : 1 week on, 1 week off (Days & Nights) ...Port Vessel Unit (PVU) Engineer required for UK Port.
Sign Up For News & Updates
- Industry Updates
- General Boating News
- Something Else
- I am happy to receive email updates from Viking Crew
- I agree to your Terms & Conditions
Ready To Apply?
Apply with 1 click with your viking crew account..
Don't have one? Click below to register and complete your profile
Email Address
Remember Me

Register With Viking
Search saved.
Manage your search preferences in your user profile
Thankyou for your message.
We aim to respond to all queries within 24 hours. Still looking for the perfect job? Start a search now
Thank you for signing up, keep an eye on your inbox. Ready to start your job search?
- Our Clients
- Our Offices
- Associations & Accreditations
- Crew Your New Build Yacht Projects
- Yacht Services Overview
- Funding and Grants
- Maritime Labour Convention (MLC)
- Green Crew Pathway
- Mental Health & Wellbeing
- Women in Maritime
- MCA Wellbeing at Sea Tool
- Newsletters

Back to Blog
Careers Engineering
Getting started as an Electro Technical Officer in Yachting 26 October 2018
I’ve had some great conversations lately with etos looking to join the yachting industry from various backgrounds, many of them have transferable skills which would be highly sought after on superyachts. i asked experienced eto jameel ‘jimmy’ rahaman to share his story about how he got started, and to provide some pointers to those considering making the move..

Nationality: Trinidadian
Qualification: CCNA, MCSE, MCSA, A+, N+, Security+, Studies in Information Sciences
When and how did you realise you wanted to become an ETO?
- After my studies in British Columbia, Canada, I returned shoreside to Trinidad & Tobago working for the largest conglomerate in the Caribbean known as the Neal and Massy group of companies. The experience gleaned from my years there cannot be overstated, but there was always a sense of fulfilment missing, an urge to explore, to push boundaries and carve before me an exciting life vs the monotony that tends to become you behind a desk. I would boldly say that the ‘Dream’ to which many believe a fallacy is what ultimately drove my decision making and eventual success in a somewhat unforgiving industry. Be the master of your fate.
How did you decide which route to go down in order to gain experience?
- This was no easy task. I began as a volunteer aboard the S/V Roseway run by the World Ocean School. Here we taught children the art of sailing around the island of St. Croix [USVI]; despite this being an unpaid position we were happy as a crew, but I knew that this would be a short-lived position having set my sights further afield. After spending six-months aboard the Roseway I returned to the shores of St. Maarten to look for day-work and begin working my way into the yachting community. I often offered help free of charge in the way of PC/Laptop repair, troubleshooting the servers of crew agencies, marina offices – Even something as simple as helping a Captain get the hang of his new phone. One hand doesn’t clap – you keep that in mind and you are well on your way to a promising start, everyone loves a smiling face with an outstretched helping hand.
How did you first hear about yachts and what made you decide this was the path for you?
- I spent much of my childhood, sailing small vessels such as Lasers and 420’s. I was a member of the 1st Presentation Sea Scouts for seven years. We often rowed old-school clinker-built pirogues on the King’s Wharf in Trinidad; racing, swimming and diving by the wrecks being the most frequent activities. Having this extensive exposure to boating kindled in me the desire to pursue more of the same, one may argue, deeper concentrations of such as it were.
What was the biggest challenge you faced when getting started in the industry?
- This would surely be that of finding a way to stand out among the plethora of yachties already fighting tooth and nail to secure their own spot aboard the next vessel hiring. You should always be willing [within reason of course] and remember to keep yourself in that state of perpetual learning. Very few of my family members were supportive of my endeavour into yachting and some would go as far to jest at my expense, I have learned that it is within the walls that hope to bind you. Finally – Humility, this is more important than most realise and is required even more so in conflict. Be the good lad.
How did you get your first yachting job?
- Day-work. I was up at ‘Smilers’ crew-house in SXM at the break of dawn (well ok, maybe 07:15) I was there with CV’s in hand and showing I was eager to offer help to anyone who even seemed remotely interested to be honest. In this industry, like many others the key is to stay hungry !
What’s your best yachting memory and why?
- My fondest memory would have to be that of my first great storm. Leaving Gibraltar, headed for Cape Verde. We were forced to leave the safety of GIB as the port authority would not tolerate us riding the storm out in the channel and we were unable to remain alongside on account of our fenders popping like balloons with our fairing taking the brunt of the damage against the quay. Unfortunately that storm rode us down to Cape Verde. For three days we suffered 9 metre waves and 80 knots of wind with gusts up to 120! The bridge wings have been breached and the sea water was covering our ankles. The Captain is not batting an eyelid but holding his own. We were heeling so badly I felt as though I had to constantly adjust my body to lean port or starboard just to stay oriented to some degree. Then to make matters worse, blackout! Deadship in the middle of the ocean and waves are having their way with us. At this stage our heeling angle is simply ridiculous for our vessel and some were bracing for that moment we would actually capsize. We had only restored power briefly before we suffered another blackout which as it would turn out be seven in total! Now, why is this my favourite memory? The way we came together as a crew behind our Captain, acting as one to overcome this storm under these frightful conditions was nothing short of astonishing. I shall always feel well grounded in any situation and I mean ANY situation as a result of the events that took place during that 72 hour period. It’s worth adding that once we made it to Cape Verde we all sat at the local pub that evening in silence, having our first pint across from one another. It felt, in a word… triumphant!
What do you like most about your job?
- I love constantly being challenged, better still, the act of overcoming them day after day. It is truly a satisfying feeling to bring calm to someone or a group of people who may otherwise feel flustered or panicked and you simply being good at your job makes all right in the world once more for a brief a moment.
Any huge disasters whilst on-board? If so, did you manage to pull it back?
- The most daunting task I had been faced with was the essential refit of the AVIT system on an 80m in 36 hours from scratch, before sailing to take a charter for a fortnight. I am pretty sure I pulled every trick in the book and then some to get this done.
What bit of kit couldn’t you live without?
- My grab bag. That’s an article all on its own but here’s a brief overview; BAHCO ratchet set, a good power tool with shaft extensions – don’t forget to keep extra batteries for it in the side pockets, 3M velcro, wire terminals [variety of sizes but smaller than not], drop-cloth and last but not least your multimeter!
What’s the best thing about working on a Superyacht?
- The friendships that you forge.
- The exposure to environments and situations that keep you on your toes forcing you to sharpen your mind to stay in the game.
- Experiencing the culture richness of yachting itself whether it be from your crew or the places you visit.
Where is the best place you have visited?
- I have to say that Argentina and Greece are my favourites. I have been from the Galapagos to the Maldives to Thailand and yet there is an uncanny charm to both Argentina and Greece that you only discover at length. To truly get my meaning you will need to let these places envelop you. Done right, you’ll emerge smiling with the morning sun, bursting at the seams with stories for your mates back home.
What advice would you give someone starting out as an ETO in the industry?
- Stay hungry !
- Every day is a school day!
- Be kind to your crew.
- Pay it forward.
If you’d like more information on ETO’s and the roles we’ve got on at the moment please don’t hesitate to contact [email protected] and register with us HERE

About the author
Guest Article: The art of ‘being human’… and keeping a happy crew
Part 2: building a good culture, keep up to date sign up to the quay crew newsletter.
I have read the Terms & Conditions and would like to be added to the mailing list
- Superyacht Recruitment Services
- Superyacht Captain Recruitment
- Partnerships
- Meet the Team
- Work for Us
- Land-based Recruitment Services
- Private Residence Recruitment Services
- Current Vacancies
- Crew Resources
- Candidate Registration
- Client Login / Register
- Candidate Login / Register
Being an ETO: The Good, the Bad and the Ugly

As an experienced superyacht ETO (Electro-Technical Officer), I wanted to share some insight into the role for anyone wanting to get into the superyacht industry.
From fixing the captain's email account to troubleshooting an engine fault, the role of an ETO is extremely broad and the job can be very fulfilling. Travelling the world and playing with the latest and greatest tech equipment is a hobby in itself, and usually a proven ETO will work towards a rotational position, typically two months on, two months off, so they can enjoy some well-earned downtime.
The position is expansive and comes with a lot of high expectations. You are responsible for the front end of the charter where you will make sure everything is in optimum condition in regards to AV/IT and electrical systems and, depending on the vessel, this usually involves interacting with guests and owners, which may have you helping guests with their movie selection or creating a video to present their latest trip. On the other side, your responsibility extends to the unseen parts of the vessel, keeping the engine room and main switchboard ticking, maintained and up to standard.
And now for the good, bad and ugly...
Job satisfaction
The job satisfaction of fixing a failed system is fantastic! Picture the following scenario: you’re called to a scene where a system is broken down, and the ship needs this particular system up-and-running asap. As an example, the X-Band Radar has failed. You start to make some logical checks, you find the fault and react by repairing it. You power on the system, and an LED begins to blink, the scanner begins to spin, the echo is now displayed on the monitor! The equipment is running as it should be - now the vessel and the captain can navigate appropriately and in a safe manner. Situations like this don't always come stress-free, and you may have a billionaire shout at you from time to time, but the best way to handle any onboard fault is to stay calm and composed. Did someone touch it? If so, they probably introduced the fault.
Getting the right crew - the pros will always show
Hiring the right crew members is vital to achieving success as an ETO. Obtain proven, tried and tested professionals who know how to manage a vessel properly. Getting on with your fellow crew members and having a positive outlook on life can go a long way in making your onboard experience more enjoyable. You need people who can follow the rules, regulations and even curfews - it can be like going back to school and, for some, this is hard to accept but it's part and parcel of being a yachtie.
It’s not all work at sea though. Sometimes it can be like living in a floating youth hostel with people from all around the world who want to work hard and play harder. It’s also a great place to get involved in water sports and fishing, and there will be plenty of fun times. Providing you perform well in your role and get along with people, you should have a job for life, working for half the year and getting to see different parts of the world.
A well-oiled team
The ETO department is part of the engine room team, but we have a unique role within that department that many people will not be familiar with. Nearly every vessel I have worked on has had the luxury of a 2nd ETO. So much more work can be achieved with two, as all menial jobs can get wrapped up instead of being added to a long list. With an extra set of hands to keep on top of the systems more efficiently, keeping documentation in order, logging the history of equipment, daily diary, and labelling and tidying up every system. There’s always plenty of work to do but there’s a middle ground somewhere between both extremes.
Crew training
I have always found a well-trained interior team to be extremely helpful to an ETO, as they can operate the AV/IT rather than seeking us out for simple tasks, which also avoids guests having to wait around unnecessarily. If the team know their way around the AV system I encourage them to use it as much as possible so they can find any potential issues before a guest gets a chance to. A well-oiled interior team goes a long way to making guests feel comfortable and in good hands as the crew appear competent and confident in what they are doing. Running a busy charter with an untrained interior team can be extremely tough, especially without a second ETO, so be fair to the crew and they will, in turn, be good to you.
Recording is essential
At the end of the day, the yacht is an amazing piece of engineering, however, it’s all about having the right crew for the boat and the owner. Without the right team, the ship can quickly spiral out of control and accidents can happen. Good crew members will make sure systems are well maintained and up to standard, safety procedures are in place, and maintenance tasks are performed regularly and recorded. It’s critical as an ETO to cover your tracks and to take videos, photos and details of your onboard systems during day to day events. Record as much as possible during shipyard periods and the build phase, as equipment may later be covered up beneath ceiling panels or walls; this evidence will be so beneficial when you have a fault or are looking to upgrade in the future.
Location-location-location?
I have worked on ships for over two decades and typically I see the same problems on every ship. One thing in particular is seeing equipment squeezed into inappropriate places - all crew members will agree with me here. This can lead to numerous headaches and can be a general hazard. Poor location can result in a lack of maintenance for the particular part; vents may get clogged with dust and equipment may overheat. I do appreciate that every square inch is important space on a yacht, but common sense should be applied when installing equipment.
The crew's personal IT guy
As the technical guy on board, some crew use ETO’s as the go-to guy for all their tech needs, relying on us to fix their personal devices. Being stuck at sea, who else do they ask right? However, ETO’s generally have enough on their plate already without the extra workload, so this can be a delicate subject. I would recommend that you trade some tasks with others and start as you mean to go on, otherwise you will have no free time to yourself, which is invaluable while you are on charter. But everyone’s different; some ETOs will mind more than others.
Passwords and credentials
There’s nothing worse than joining a boat to find out there is no password organisation, and you have to struggle to log in to various accounts. Working off a scratchy notebook that’s been passed around, or a badly organised spreadsheet can turn a simple task into a nightmare. I would recommend using a password management system with 2-factor authentication for all your usernames and passwords.
Documentation
This applies to drawings and documentation records. I cannot stress enough how important it is to get these in a logical order. Let’s not worry what the previous occupants should have done; it’s our mission to leave the boat a better place than we found it. The ETO world is tiny and you are only as good as your last job, so it’s best to leave it in tip-top condition to maintain a good reputation. Some may argue: ‘well that’s how I found it’ or ‘why should I make it easier for my replacement when I leave.’ What goes around comes around and bad news travels quickly in this small industry, so it’s best to give it your all and be remembered as a good ETO instead of an average one.
Knowledge is power
In contrast to supporting the next crew on board a vessel, some individuals will actually withhold information to make themselves look better (including chief engineers, captains and even your back to back ETO partner). This is the mindset of insecure individuals who just look after themselves. We are a team on board, and it’s our task to make our crew and our rotational partner's life more comfortable by passing on information. Never go down to their level, they will get found out one day. Keep doing a good job, record what you do and be totally transparent, and you won’t go far wrong.
Inheriting a can of worms
So you nailed the interview and you have been selected for a new role as an ETO on board a vessel. Great!, you start your new role on the superyacht full of hope, and then bang...reality kicks in. You find out the vessel has been poorly looked after and neglected for years. Unfortunately, we see this time and time again. The owner doesn’t want to spend money on the right personnel or maintenance costs, or contemplate the price of an upgrade. But the ship is only as good as the crew and management maintaining her, so scrimping on salaries will only lead to the yacht getting a lower standard of ETO. The owner gets what they pay for.
Pick the right battles
Be sure not to get bogged down with low priority tasks for too long; these little tasks can grab your attention and make you lose focus on what really matters and what you are responsible for. I once faced this scenario when I joined a boat and the radio room had issue after issue. I decided enough was enough and I was going to rewire all of the equipment as it was spaghetti junction behind the panels. I started to rewire, making progress, then out of nowhere we lost the entire AV system! I couldn’t be in two places at once...It wasn't an option to leave the AV therefore I had to sacrifice the radio room. This fault took me a day to resolve which meant I left the radio room compromised and not functioning. Fortunately we didn't sail anywhere, but what if we had? I would have been screwed! That left a big impression on me and from that day I changed my mentality.
Excessive firefighting
One of the ETO’s worst nightmares is working with a poorly installed AV system and firefighting from room to room fixing fault after fault. Your AV system is at the very front end of the charter, controlled by your owners and guests. It is paramount for the entire charter that the system is bulletproof and performing as it is intended to. I have seen many new and old installations where lots of cables are underrated, joined unnecessarily and bent over excessively. It can seem like there's a different set of rules for some of these AV guys who install pieces of equipment versus a good marine electrician. As a rule of thumb to the untrained eye, if the install looks neat, then the contractor generally cares, and you are probably in for a sound system which is highly dependable.
Babysitting
Some systems need babysitting and constant attention because they are not reliable. AV systems generally have this reputation but you will always get a ‘clever guy’ that comes along and says “did you turn it off and on?”. This type of advice is all too familiar, and it gives the AV/IT guys a bad rep because rebooting equipment does work a lot of the time….However, you still need to know what to reboot in the first place. Ideally, nobody wants to reboot a device at all, as a system should run flawlessly, but this will never be the case as processors on board will always need a little tickle now and again.
We are employed as ETOs to keep the on board tech systems running and to react whenever there is an issue. Sometimes this means working under pressure in front of the owner/charter guests/captain to get the radar back on asap, which is unfortunate. I always say that if you were in a hotel room, you wouldn’t want an AV guy coming in, taking your TV off the wall and troubleshooting why there is an issue. Still, sometimes you may not have a choice, and you have to do what’s necessary to get the job done.From experience, I would say that if you show yourself as proactive and trying your best, then usually the boss will be ok with the odd invasion of space.
Suppose you have been dealt a weak hand with your AVIT setup. In that case, it’s best to prioritise the most critical systems which affect your charter, patch them up where possible and plan ahead to install them properly whenever possible.
The ETO is in good part responsible for the safety of electrical systems and the maintenance of the navigation systems on board a vessel. Sometimes we look like superheroes, other times we look like the devil because it’s ‘our’ system that failed. Most of the time, the role of a superyacht ETO has a real feel-good factor about it - every day is a school day on board, no matter how experienced you are and, if you're lucky, you'll get to operate some of the latest generation technology. Most of all, having the right crew is essential for a successful charter and even if they don’t always come cheap, they will be worth their weight in gold.

Post your comment
You cannot post comments until you have logged in.
Comment by: Merah Putih - 15 Oct 2020, 01:39 (4 years ago)
Amazing jobs..bro....
No one has commented on this page yet.
RSS feed for comments on this page | RSS feed for all comments
Search articles with keywords

Electrical and Technical Officer
The ETO works closely with the captain and other crew members to ensure that all systems are in proper working order and to troubleshoot and repair any issues that arise. They also may have a role in the maintenance and repair of the yacht’s interior and exterior systems, such as air conditioning, lighting, and audio-visual equipment.
How to Become an ETO on a Yacht
To become an ETO on a superyacht, you will typically need to have a strong background in electrical, electronic, and mechanical systems, as well as experience working on marine vessels. The following are some steps you may take to become an ETO:
- Education: Obtain a degree in marine engineering or a related field, such as electrical or mechanical engineering.
- Certification: Obtain relevant industry certifications, such as a Y4 or Y3 engineer certification or an advanced marine engineering diploma.
- Experience: Obtain experience working on marine vessels, either through internships, apprenticeships, or work as a deckhand or engineer on smaller vessels.
- Training: Complete additional training courses, such as safety and survival training, first aid, and firefighting.
- Networking: Build a network of contacts in the maritime industry to learn about job opportunities and gain experience.
- STCW: Obtain an STCW (Standards of Training, Certification and Watchkeeping) certification, which is an international standard that sets out basic safety training and qualifications that all seafarers must have.
It is important to note that most superyachts have a high standard of safety and security, and many will require their crew members to have specific certifications and credentials, such as STCW, as well as a certain level of experience before being hired.
Yacht ETO FAQs
What are the qualifications and experience required to be an ETO on a superyacht?
A minimum of a Y4 or Y3 engineering certification is typically required, along with experience in marine engineering.
Knowledge of and experience with electrical and technical systems on large vessels is also essential.
Some employers may require additional certifications such as STCW95 and a valid passport.
What are the main responsibilities of an ETO on a superyacht?
The ETO is responsible for maintaining and managing all of the electrical and technical systems on the yacht, including generators, air conditioning, water systems, and navigation equipment.
The ETO also manages and oversees the maintenance of all technical equipment and supplies on the yacht.
The ETO is also responsible for ensuring compliance with all maritime regulations and safety standards.
How does the ETO interact with the rest of the crew and guests?
The ETO works closely with the captain and other crew members to ensure the smooth operation of the yacht.
The ETO may also interact with guests to provide technical support or troubleshoot any issues that may arise.
How does the ETO manage and maintain the electrical and technical systems on the yacht?
The ETO conducts regular inspections and maintenance on all electrical and technical systems to ensure they are in proper working order.
The ETO also keeps detailed records of all maintenance and repairs.
The ETO troubleshoots and repairs any issues that may arise with the systems.
What is the typical schedule of an ETO on a superyacht?
An ETO typically works a rotational schedule, which can include extended periods of time at sea.
The ETO may also be required to be on call to handle any issues that may arise with the technical systems.
How does the ETO handle emergencies or equipment failures in the technical systems?
The ETO should have a good understanding of the yacht’s technical systems and be able to troubleshoot and repair issues as they arise.
The ETO should also be familiar with the procedures for handling emergencies and equipment failures.
What are the everyday challenges of being an ETO on a superyacht?
Being away from family and friends for long periods of time can be challenging for some ETOs.
The ETO may also face challenges with managing and maintaining equipment in a marine environment.
The ETO may also have to troubleshoot and repair equipment in remote locations.
How does the ETO handle budget and inventory management for technical equipment and supplies?
The ETO is responsible for managing the budget for technical equipment and supplies, which includes ordering and stocking parts.
The ETO also keeps track of inventory and ensures that the yacht has enough supplies on board to handle any repairs or maintenance that may be needed.
What is the typical salary range for an ETO on a superyacht?
The typical salary range for an ETO on a superyacht is between €6,000-€8,000 per month
Salary can vary based on the size of the yacht and the ETO’s level of experience.
ETO Jobs Available
© 2024 All rights reserved
Privacy Overview
- Engineering
Electrical Technical Officer (ETO)
Best Match Date Added (Latest First) Start Date Salary (High to Low)
Please select the options to filter jobs & positions
Job Type Any Permanent Position Rotational Contract Seasonal Temporary Daywork Cruising Delivery Mile Building Ocean Sailing Sail Racing
Department Any Accounting & Finance Administration & Clerical Build & Refit Creative & Marketing Crew Placement & Services Crew Training Deck Directors Engineering Galley Interior IT & Operations Specialist Yacht Management Yacht Sales & Charter
Position Any Fleet Captain Build Captain Captain Skipper Chase Boat Captain Relief Captain Chief Officer/1st Mate Deckhand/Mate 2nd Officer 3rd Officer Bosun Lead Deckhand Deckhand Deckhand/Security Junior Deckhand Deck/Steward(ess) Deck/Engineer Deck/Carpenter Deck/Divemaster Competent Crew Delivery Crew Dayworker Race Crew (Professional) Race Crew (Amateur) Chief Engineer Relief Chief Engineer Sole Engineer 2nd Engineer 3rd Engineer Chief ETO (CETO) Electrical Technical Officer (ETO) Electro-Technical Rating (ETR) AV/IT Officer Storekeeper Engineer Motorman Wiper/ Oiler Tender Engineer Junior Engineer Executive/Head Chef Sole Chef Sous/2nd Chef Chef de Partie/3rd Chef Commis/4th Chef Cook/Crew Chef Cook/Steward(ess) Purser Concierge Household/ Estate Manager Chief Steward(ess) Interior Manager Head of Service Head of Housekeeping Spa Manager Spa Therapist/ Steward(ess) Butler Sole Steward(ess) 2nd Steward(ess) 3rd Steward(ess) Steward(ess) Service Steward(ess) Sommelier Housekeeping Steward(ess) Laundry Steward(ess) Junior Steward(ess) Stew/Masseur(euse) Host(ess) Private Security Officer (PSO) Close Protection Officer (CPO) Private Driver/ Chauffeur Helicopter Pilot Helicopter Mechanic Hairdresser/ Barber Beautician Masseur(euse) Governor/ Governess Nanny Au Pair Tutor Florist Personal Assistant (PA) Executive Assistant (EA) AV/IT Specialist Videographer Personal Trainer (PT) Yoga/Pilates Instructor Sub-Pilot Dive Instructor Watersports Instructor Doctor Nurse Paramedic Chairman Chief Executive Officer (CEO) Group Financial Controller (GFC) Chief Financial Officer (CFO) Managing Director Director Financial Director Technical Director Training Director Yacht Management Director Charter Management Director Yacht Charter Director Yacht Sales Director Operational Director Company Secretary Fleet Protocol Director Maritime Compliance Director Creative & Marketing Director Yacht Sales Broker Yacht Charter Broker Charter Manager Charter Accounts Manager Charter Accounts Support Yacht Market Analyst Sales & Product Marketing Manager Sales & Product Marketing Assistant Sales Manager Senior Sales Executive Sales Executive Head of Yacht Management Yacht Manager Operational Manager Client Relations Manager Insurance Manager Insurance Consultant System Development Crew Compliance Manager Yacht & Crew Compliance Crew Compliance Administrator Crew Compliance Support Crew Services Administrator Head of Maritime Compliance & DPA Marine Superintendent Maritime Compliance & DPA Maritime Solicitor Marina Manager Marina Operative DPA & Safety Manager Yacht Compliance Manager Yacht Compliance Administrator Yacht Compliance Support Head of Yacht Accounts Lead Yacht Accounts Yacht Accounts Manager Yacht Accounts Administrator Yacht Accounts Support Fleet Technical Manager Project Manager Project Engineer Project Coordination Project Controller Supply Chain Manager Environmental Manager Supervisor/ Foreman Naval Architect Mechanical Engineer Marine Engineer Marine Electrical Engineer Marine Technician 3D CAD Technician/ Modeller Concept Designer (creative) Detail Designer Design & Proposal Engineer Design Engineer Senior Interior Designer Structural Engineer Interior Designer Cost Estimator Technical Superintendent Technical Manager Technical Controller Technical Assistant Technical Financial Controller Procurement Manager Procurement Assistant Head of Technical Compliance & DPA Logistics Project Manager Materials Controller Yacht/ Boat Builder Marine Joiner/ Carpenter Mechanical Fitter Marine Electrician Marine Plumber/ Pipefitter Marine Surveyor Sprayer/ Painter Laminator/ Finisher Assembler/ Fabricator Slinger (crane & lifting operative) Sail/ Cover Maker Upholsterer Seamstress Welder/ Plater Shipyard/ Warehouse Operative CNC Operative Corporate Development Manager Marketing Manager Marketing Executive Marketing Assistant Yacht Marketing Graphic Designer Content Writer Creative & Events Digital Marketer & SEO Partnerships Liaison PR & Communications Officer Head of Client Relations Head of Information Technology (IT) Business Development Manager IT Support Technician Web Designer/ Developer Crew Manager Recruitment Consultant Crew Assistant Crew Employment and Payroll Manager Crew Employment and Payroll Administrator Training & Exam Coordinator Training Coordinator Head of Safety Training Instructor Company Secretary Office Manager Listings Manager Administrator Customer Service Office Support/ Assistant Personal Assistant (PA) Executive Assistant (EA) Human Resources Manager Human Resources Administration Human Resources Support Group Finance Controller Assistant Group Finance Controller Finance Manager Financial Administrator Financial Analyst Accountant/ Book-keeping Accounts Administration
Team / Couple Don't mind Yes No
Vessel / Shore Based Type Any Chase Boat Commercial Vessel Expedition Vessel Fishing Vessel Motor Yacht Research Vessel Sailing Yacht Shore Based Position
Vessel Size Any 0 - 30m 31 - 39m 40 - 49m 50 - 74m 75 - 94m 95m+
Salary (e.g. £, $, €) Any 0 - 1,500 1,501 - 3,000 3,001 - 5,000 5,001 - 10,000 10,001 - 15,000 15,000+ per month per day
Location Any Antigua & Barbuda Australia France Greece Italy Monaco Seychelles Spain United Arab Emirates United Kingdom United States Virgin Islands (British) Virgin Islands (U.S.) Bahamas Bahrain Barbados Canada Cape Verde China Croatia Cyprus Egypt Fiji Finland French Polynesia Germany Gibraltar Hong Kong Indonesia Malaysia Maldives Malta Mexico Montenegro Netherlands New Zealand Oman Philippines Portugal Qatar Saudi Arabia Sint Maarten South Africa Sweden Switzerland Thailand Turkey
Keyword Search
Clear all filters

- 9 positions

We are Yotspot
The leaders in superyacht recruitment

- Job ID #2329450
- 80m (262ft) Motor Yacht
- Starting 5th Jun 2024
- Posted Yesterday

- Job ID #2329204
- 90m (295ft) Motor Yacht
- Starting 1st Jun 2024

- Job ID #2329144
- 78m (256ft) Motor Yacht
- EUR (€)7,000.00 Per Month

- Job ID #2327759
- 75m (246ft) Motor Yacht
- Starting 4th Jun 2024
- EUR (€)465.00 Per Day
- Posted 28th May 2024
- Job ID #2324277
- 105m (344ft) Motor Yacht
- Starting 28th May 2024
- Posted 25th May 2024

- Job ID #2324511
- 100m (328ft) Motor Yacht
- Posted 23rd May 2024
- Job ID #2321329
- 120m (394ft) Motor Yacht
- Starting 21st May 2024
- EUR (€)8,820.00 Per Month
- Posted 21st May 2024

- Job ID #2257315
- Location Oundle Salary £25 per hour Job type ...
- Posted 18th Mar 2024
Electrical Technical Officer (ETO) Position Filled
- Job ID #2307892
- Starting 16th Sep 2024
- EUR (€)6,000.00 Per Month
- Posted 20th May 2024
This role is normally found on larger super yachts where there are a big team of engineers. They are responsible for all electrical equipment such as computers, GPS, navigational equipment to TVs, Internet and computers.
Salary range
EUR 4500 to EUR 6000+ Per Month
Qualifications, training and skills required
- Prior experience with AV/IT equipment
- Any qualifications in electronics will be advantageous
- Training in computer repairs, televisions and Internet, radar and navigation equipment, communication equipment such as satellites, phones and radios
- STCW basic crew training
- ENG1/ML 5 Medical Fitness Certificate
- MCA Engineering certification
Extra desired training
- New build experience
- Foreign language skills
Engineer Careers Advice
Thinking of working as a yacht engineer.
To put it simply, the Yacht Engineers keep the boat going, keep the water clean, the lights on, the wifi working, and just about anything you can think of! This covers all areas of mechanical and electrical maintenance, upgrade, and repair. Engineers will typically have routine maintenance and checks depending on the operation of the vessel, as well as responding to failures, breakdowns, and emergencies. The Engineering team is a crucial part of emergency response, managing power generation and water pumping.
Below we outline the various roles, responsibilities, and qualifications necessary to become a Yacht Engineer.
Yacht Engineer Job Roles
Essential skills and experience.
Chief Engineer is responsible for the overall condition of the onboard systems, reporting to the Captain. S/he is required to manage teams of up to 15 people. Chief Engineer will typically be required to plan maintenance periods in accordance with class society requirements.
Qualifications
Depends on the combined propulsion power and Gross Tonnage of the vessel. For larger yachts, a Chief Engineer Unlimited CoC will be required. High Voltage qualifications, and experience with new build projects is often desirable.
Must be a good thinker. Good with your hands, and not afraid of dirty or malodourous tasks! The engineering team work best as a team, with everyone taking responsibility for the team. Dedication to the task, and an understanding of the importance of the role in keeping the rest of the vessels’ crew and guests safe.
If going down the ETO route, there is a case for getting your ETO CoC III/6 as you will be working with HV and can be signed on as an ETO for manning requirements. Good electrical background or degree will also be highly advantageous. With AVIT there are a number of courses that would be useful, mainly the Cisco CCNA, Crestron CTI, Microsoft Courses and CompTIA, Level 1 and 2 courses from providers like SEA Certify (Just ETOs) and Bond TM. Any cybersecurity qualifications are a bonus too.
A good background in AVIT installation or management is also beneficial. Troubleshooting and having fast answers are crucial when dealing with owners and guests. Due to this a strong and friendly personable manner are crucial as you will be face to face with HNWI frequently.
More Yacht Engineering Advice
A day in the life: yacht av/it engineer, how to become a yacht engineer – qualifications and requirements, lithium ion batteries – friend or foe, we’re here to help.
Elan House, 5a Little Park Farm Road, Fareham, Hampshire PO15 5SJ
You are using an outdated browser. Please upgrade your browser to improve your experience.

New job for ETO on Mega Yacht
An experienced ETO is required to join a 100M+ M/Y ASAP.
Applicants must have prior experience in a similar role aboard yachts / passenger ships.
The minimum certification needed would be: STCW, ENG1, ETO COC, DSD and High Voltage
On offer is a Euro salary and 182 days paid leave per year (3:3)
Apply at: bit.ly/2JhCha5
Shop for mariners

© The Electro Technical Officer (ETO) | Disclaimer | Terms of Use | Privacy Policy | FAQ
Privacy Overview
Necessary cookies are absolutely essential for the website to function properly. This category only includes cookies that ensures basic functionalities and security features of the website. These cookies do not store any personal information.
Any cookies that may not be particularly necessary for the website to function and is used specifically to collect user personal data via analytics, ads, other embedded contents are termed as non-necessary cookies. It is mandatory to procure user consent prior to running these cookies on your website.
Yacht Crew Job Board
With Bluewater's expertise in crew training and yacht crew recruitment, finding your ideal yacht crew vacancy is simple. We offer yacht management services to a variety of exclusive superyachts. Our team excels in sourcing top-notch yacht crew positions, spanning from 25-meter private yachts in the Bahamas to 50-metre charter yachts in the Mediterranean to luxurious 100+ metre superyachts navigating the globe extensively.
78 yacht crew jobs available now.
Yacht Crew Training
Alongside sourcing the latest yacht crew jobs worldwide, Bluewater offers a range of specialised yacht crew training courses. Whether you're new to the superyacht industry seeking entry-level qualifications, an experienced deckhand or engineer aiming to advance your career, or a dedicated crew member looking to enhance your resume with certifications like HELM (Human Element Leadership and Management), Yachtmaster, or OOW (Officer of the Watch), explore our comprehensive yacht crew training options.
Working on a Luxury Yacht
Working as a crew member on a superyacht is undeniably one of the most rewarding yet demanding professions, calling for hard work, dedication, and professional training. The opportunities within the yachting industry are vast, and at Bluewater, we are committed to helping every crew member discover their ideal yacht crew position. Our recruitment division focuses on finding the perfect yacht for crew members and provides unparalleled professional support. Our recruitment experts guide crew members through every step of their yachting career journey, ensuring they receive the best possible assistance.
Manage Your Yacht Career
Whether you're seeking a yacht crew position as a deckhand, engineer, onboard masseuse, stewardess, chef, chief stewardess, purser, first officer, or captain, take control of your yacht career. Create a profile and join one of the world's largest yachting communities for free.
78 JOBS FOUND
- Qualifications: AEC2 minimum, at least some Y4 modules.
- Experience: 2+ years
- Salary: €6000 & good package
- seasonal to permanent if happy
- Qualifications: STCW, ENG1 AEC2
- Experience: 1- 2 years
- Salary: tbc

- Qualifications: Yachtmaster Offshore, Dive Instructor
- Experience: 2 Years +
- Salary: TBC
- seasonal until October
- Qualifications: STCW95 ENG1
- Experience: 1 year+
- until the end of Sept, mid October
- Qualifications: STCW, ENG1
- Experience: 1 season
- Salary: €3000
- Qualifications: STCW, ENG1, Food & Hygiene Level 2
- Experience: 5 Years +
- Salary: DOE
- Qualifications: Master 200gt
- Experience: 3+ years
- Salary: 5-6000 euros
- Qualifications: Yachtmaster Offshore
- Experience: 2 to 3 Years +
- Salary: 4500EUR
- permanent 5:1
- Qualifications: STCW, ENG1,PDSD
- Salary: 2800
- Michigan News
- National News
- International News
- Local Sports
- Michigan Sports
- National Sports
- Editorials and columns
- Letters to the Editor
- Engagements
- Anniversaries
- Coronavirus
- Classifieds
- Garage Sales
- Submit News
- Statement of Values
- Terms of Service
- Browse Notices
- Place Notice
- Today's Paper
Subscribe Today
Fireside 500 stock outboard races this weekend at grand lake.

Courtesy Photo by Eugene Cambre Racers take off in the 2023 Fireside 500 marathon on Grand Lake. Races will be held Saturday and Sunday, starting from The Fireside Inn. Spectators are welcome at this free event.
PRESQUE ISLE — Presque Isle Yacht Club, in association with Top O’ Michigan Outboard Racing Club, presents the Fireside 500 Stock Outboard Race on Saturday and Sunday at The Fireside Inn.
Racing starts at 10 a.m. on Saturday, featuring the Eastern Marathon Championships, Short Course, J Marathon, and Short Marathon. Awards will be presented at 5 p.m. Then on Sunday, racing starts at 10 a.m., featuring the Central Division Marathon, Short Course. Awards will be at 4 p.m. on Sunday.
These events are free to spectators and open to the public.
The Fireside 500 started in 2019. This will be the fifth year of the event, as it was paused during the pandemic.
Mike Bugenske, Dave Kowalski, and Terry McConnell of Presque Isle Yacht Club Events Inc. started the event, teaming up with Race Director Tom Fairbairn from Top O’ Michigan, and Alan McConnell and Lori VanSchoten of Fireside Inn.
“The racers love it, because they can come and keep their equipment on site, they can rent rooms and cabins, they can get their meals here, and they don’t have to drive miles and miles. It’s just the perfect setup. Grand Lake is the perfect lake to have it on.”
He said spectators will enjoy watching the race, as well. He encourages people to come out for the marathon, and other races.
“When they take off, the sound, it’s just awesome,” Bugenske said. “It’s pretty exciting.”
Fireside Inn is the place to be for spectators, he added. There will be food available, and plenty of fun for all ages.
The racers come from all over the Midwest. One racer might be in three or four events.
The weekend weather forecast is favorable so far, with 60s, sunny, and light wind, Bugenske said.
People should park on Grand Lake Road, and golf cart shuttles will be offered.
Kowalski is also the Presque Isle Harbor Wooden Boat Show chairman. That will take place on June 15 at Presque Isle Harbor, 5462 E. Grand Lake Road, Presque Isle. For more information about the 31st annual boat show, visit presqueisleharborwoodenboatshow.com.
Today's breaking news and more in your inbox
- Daily Newsletter
- Breaking News

YAC Day raises over $39K for youth

Thunder Bay Folk Society Spring Fling Saturday in Ossineke

Immanuel students enjoy petting zoo

Mike Arzo donates toys, Arzo Amusement Park passes to graduating kindergartners
Police blotter: alcona county deputies handle 107 complaints.
Recent actions by law enforcement agencies in Northeast Michigan. This has been only lightly edited. ALCONA ...
Starting at $2.99/week.
Billionaires like Jeff Bezos and Mark Zuckerberg spend six figures a year maintaining their superyachts. Here's how.
- Superyachts are one of the most expensive assets money can buy.
- The true cost of ownership is even more, adding up to millions a year.
- Here's how much it costs to own a superyacht — and what that money is going toward.
Financial advisors are quick to warn prospective owners that a boat is nothing more than a hole in the water in which to throw money. When it comes to superyachts , you'd better have bags and bags of cash.
As one luxury agent told Business Insider at the Palm Beach International Boat Show: "Buying a boat, it's a huge purchase — and nobody needs a yacht."
A superyacht, generally over 30 meters long, is one of the most expensive assets money can buy, with the largest costing more than a lot of real estate or a private jet. Billionaires like Jeff Bezos, Mark Zuckerberg, and Steve Jobs each spent nine figures on their megayachts.
That doesn't include operating costs. Owners should expect to pay about 10% of a yacht's new-build price each year, experts told Business Insider. That's tens of millions of dollars annually for the most luxurious boats.
"It's a small-to-medium-sized business in its own right," said Jeffrey Beneville, a senior vice president at insurance company NFP, where he specializes in consulting clients about yachts.
Unlike many smaller boats, superyachts need staff, not just a captain. Some superyachts have space for dozens of crewmembers , including a chef, engineer, and masseuse for the guests onboard. Each gets an annual salary — the highest-ranking members earn six figures — and benefits. Eric Schmidt's yacht fits a crew of 28 for a ratio of about two crewmembers per guest.
Then there's fuel, dockage fees, routine maintenance, and insurance. The latter hinges on everything from the reputation of a yacht's shipyard to where an owner wants to take it (if a vessel is taking frequent trips to the South China Sea, for example, expect to pay a higher premium). If a superyacht has a support yacht — or a support superyacht, in Bezos ' case — expect to pay another 10% of that boat's price annually.
"The cost to maintain a yacht is so high that they just think that money's getting lit on fire," Matthew Fleissig, the CEO of wealth management firm Pathstone, told BI of his clients who choose to charter rather than own.
One of his firm's clients who does own has a 23-meter yacht valued at $5.2 million. The annual cost to staff, maintain, dock, and insure the boat is $346,297, according to documentation provided to BI. The lion's share is spent on marina fees ($95,970) and maintenance work ($88,408.) While not exactly a Sunfish, that boat is too small to count as a superyacht.
At 106 meters, the Amadea, owned by a sanctioned Russian oligarch , definitely does. The $300 million yacht, which was seized in 2022 and is docked in San Diego, cost $922,000 a month to maintain, a court filing showed: $360,000 for crew salaries, $75,000 for fuel, $144,000 for insurance, $178,000 in dry-docking fees, and $165,000 for maintenance, waste removal, food for the crew, and miscellaneous expenses.
"And that's an inactive yacht that's in the water," NFP's Beneville said.
If it were operational and carrying guests, the costs would be about twice that, or between $20 million and $30 million a year, he added.
Of course, it makes more financial sense for the non-obsessives to charter, and many of Fleissig's clients do. And some owners choose to offer their yachts for charter — the most luxurious cost as much as $1 million a week — to offset the costs.
"If you charter the boat for 50 days a year, it's going to help a lot," Anders Kurtén, the CEO of brokerage firm Fraser Yachts, told BI.
Then again, the running costs don't matter as much at a certain point. "If you're worth $30 billion, it's nothing. And if you're worth $117 billion — and these are the guys we're talking about — they're in it as long as it's still enjoyable for them," Beneville said. "It's not a money thing."
Watch: Why South Sea pearls are so expensive
- Main content
- Yekaterinburg
- Novosibirsk
- Vladivostok

- Tours to Russia
- Practicalities
- Russia in Lists
Rusmania • Deep into Russia
Out of the Centre
Savvino-storozhevsky monastery and museum.

Zvenigorod's most famous sight is the Savvino-Storozhevsky Monastery, which was founded in 1398 by the monk Savva from the Troitse-Sergieva Lavra, at the invitation and with the support of Prince Yury Dmitrievich of Zvenigorod. Savva was later canonised as St Sabbas (Savva) of Storozhev. The monastery late flourished under the reign of Tsar Alexis, who chose the monastery as his family church and often went on pilgrimage there and made lots of donations to it. Most of the monastery’s buildings date from this time. The monastery is heavily fortified with thick walls and six towers, the most impressive of which is the Krasny Tower which also serves as the eastern entrance. The monastery was closed in 1918 and only reopened in 1995. In 1998 Patriarch Alexius II took part in a service to return the relics of St Sabbas to the monastery. Today the monastery has the status of a stauropegic monastery, which is second in status to a lavra. In addition to being a working monastery, it also holds the Zvenigorod Historical, Architectural and Art Museum.
Belfry and Neighbouring Churches

Located near the main entrance is the monastery's belfry which is perhaps the calling card of the monastery due to its uniqueness. It was built in the 1650s and the St Sergius of Radonezh’s Church was opened on the middle tier in the mid-17th century, although it was originally dedicated to the Trinity. The belfry's 35-tonne Great Bladgovestny Bell fell in 1941 and was only restored and returned in 2003. Attached to the belfry is a large refectory and the Transfiguration Church, both of which were built on the orders of Tsar Alexis in the 1650s.

To the left of the belfry is another, smaller, refectory which is attached to the Trinity Gate-Church, which was also constructed in the 1650s on the orders of Tsar Alexis who made it his own family church. The church is elaborately decorated with colourful trims and underneath the archway is a beautiful 19th century fresco.
Nativity of Virgin Mary Cathedral

The Nativity of Virgin Mary Cathedral is the oldest building in the monastery and among the oldest buildings in the Moscow Region. It was built between 1404 and 1405 during the lifetime of St Sabbas and using the funds of Prince Yury of Zvenigorod. The white-stone cathedral is a standard four-pillar design with a single golden dome. After the death of St Sabbas he was interred in the cathedral and a new altar dedicated to him was added.

Under the reign of Tsar Alexis the cathedral was decorated with frescoes by Stepan Ryazanets, some of which remain today. Tsar Alexis also presented the cathedral with a five-tier iconostasis, the top row of icons have been preserved.
Tsaritsa's Chambers

The Nativity of Virgin Mary Cathedral is located between the Tsaritsa's Chambers of the left and the Palace of Tsar Alexis on the right. The Tsaritsa's Chambers were built in the mid-17th century for the wife of Tsar Alexey - Tsaritsa Maria Ilinichna Miloskavskaya. The design of the building is influenced by the ancient Russian architectural style. Is prettier than the Tsar's chambers opposite, being red in colour with elaborately decorated window frames and entrance.

At present the Tsaritsa's Chambers houses the Zvenigorod Historical, Architectural and Art Museum. Among its displays is an accurate recreation of the interior of a noble lady's chambers including furniture, decorations and a decorated tiled oven, and an exhibition on the history of Zvenigorod and the monastery.
Palace of Tsar Alexis

The Palace of Tsar Alexis was built in the 1650s and is now one of the best surviving examples of non-religious architecture of that era. It was built especially for Tsar Alexis who often visited the monastery on religious pilgrimages. Its most striking feature is its pretty row of nine chimney spouts which resemble towers.

Plan your next trip to Russia
Ready-to-book tours.
Your holiday in Russia starts here. Choose and book your tour to Russia.
REQUEST A CUSTOMISED TRIP
Looking for something unique? Create the trip of your dreams with the help of our experts.
health assessment research definition
- Open access
- Published: 09 June 2003
The Stanford Health Assessment Questionnaire: Dimensions and Practical Applications
- Bonnie Bruce 1 &
- James F Fries 1
Health and Quality of Life Outcomes volume 1 , Article number: 20 ( 2003 ) Cite this article
132k Accesses
483 Citations
9 Altmetric
Metrics details
The ability to effectively measure health-related quality-of-life longitudinally is central to describing the impacts of disease, treatment, or other insults, including normal aging, upon the patient. Over the last two decades, assessment of patient health status has undergone a dramatic paradigm shift, evolving from a predominant reliance on biochemical and physical measurements, such as erythrocyte sedimentation rate, lipid profiles, or radiographs, to an emphasis upon health outcomes based on the patient's personal appreciation of their illness. The Health Assessment Questionnaire (HAQ), published in 1980, was among the first instruments based on generic, patient-centered dimensions. The HAQ was designed to represent a model of patient-oriented outcome assessment and has played a major role in many diverse areas such as prediction of successful aging, inversion of the therapeutic pyramid in rheumatoid arthritis (RA), quantification of NSAID gastropathy, development of risk factor models for osteoarthrosis, and examination of mortality risks in RA.
Evidenced by its use over the past two decades in diverse settings, the HAQ has established itself as a valuable, effective, and sensitive tool for measurement of health status. It is available in more than 60 languages and is supported by a bibliography of more than 500 references. It has increased the credibility and use of validated self-report measurement techniques as a quantifiable set of hard data endpoints and has contributed to a new appreciation of outcome assessment. In this article, information regarding the HAQ's development, content, dissemination and reference sources for its uses, translations, and validations are provided.
Why assess Health-Related Quality of Life with the Health Assessment Questionnaire (HAQ)?
The ability to effectively measure health-related quality-of-life longitudinally is central to describing the impacts of disease, treatment, or other insults, including normal aging, upon the patient. Assessing these outcomes requires instruments that are comprehensive, reliable, valid, responsive, and those that have been stable for a sufficient length of time to permit longitudinal study. Such measures are particularly significant in studies where short term results are not the primary outcomes of interest, but can be of use over periods as short as six weeks.
The HAQ is one of the most widely used comprehensive, validated, patient-oriented outcome assessment instruments. It has been administered by the Stanford Arthritis, Rheumatism, and Aging Medical Information System (ARAMIS) more than 200,000 times to assess clinical status, evaluate effectiveness in clinical and observational trials, and to define health outcomes, and it is sanctioned by the American College of Rheumatology for assessing physical function in rheumatoid arthritis trials[ 1 , 2 ]. It is available in more than 60 languages and is supported by a bibliography of more than 500 references.
What is the HAQ?
The HAQ is one of the first instruments deliberately designed to capture prospectively and by protocol the long term influence of multiple chronic illnesses and to allow supplementation by additional measures for particular studies. The HAQ has played an influential role in establishing health outcome assessment as a quantifiable set of reliable, valid and responsive hard data points.
Because the HAQ emanated from the rheumatology field, it sometimes has been characterized as a "disease-specific" instrument rather than having been adjudicated on the basis of its structure, content, and history of use. The HAQ has been and continues to be administered across diverse disciplines and in different cultures, with properly designed adaptations that do not impact its reliability and validity. It should be considered a "generic" rather than a "disease-specific" instrument, since it assesses the dimensions of death, disability, drug side effects, discomfort, and economic costs, none of which are "disease-specific".
What areas of health does the HAQ measure?
The HAQ is typically used in one of two formats. The full HAQ collects data on five generic patient-centered health dimensions: (1) to avoid disability; (2) to be free of pain and discomfort; (3) to avoid adverse treatment effects; (4) to keep dollar costs of treatment low; and (5) to postpone death [ 3 – 6 ]. It includes sections on drug side effects and medical costs, as well as supplemental sections on demographics, lifestyle and health behaviors. However, the version that has received the widest attention, most frequent use, and what is commonly referred to in the literature as "the HAQ," is the "short" or "2-page" HAQ. The 2-page HAQ contains the HAQ Disability Index (HAQ-DI), the HAQ visual analog (VAS) pain scale, and the VAS patient global health scale; [see Additional file: 1 HAQ Questionnaire.pdf for a copy of the English version of the questionnaire].
As with any instrument, the HAQ has limitations, and as generally used, does not capture disability associated with sensory organ dysfunction or psychiatric dysfunction and does not directly measure patient satisfaction or social networking. Yet these variables, or other variables of interest to the user, can be readily appended.
The HAQ Disability Index (HAQ-DI). The disability assessment component of the HAQ, the HAQ-DI, assesses a patient's level of functional ability and includes questions of fine movements of the upper extremity, locomotor activities of the lower extremity, and activities that involve both upper and lower extremities. There are 20 questions in eight categories of functioning which represent a comprehensive set of functional activities – dressing, rising, eating, walking, hygiene, reach, grip, and usual activities. The stem of each item asks over the past week "Are you able to …" perform a particular task. The patient's responses are made on a scale from zero (no disability) to three (completely disabled). Each category contains at least two specific component questions (See Additional File 1_2-page HAQ Questionnaire.pdf for a copy of the English version of the HAQ-DI).
The HAQ VAS Pain Scale. The HAQ pain scale is designed to assess the presence or absence of arthritis-related pain and its severity. The objective is to obtain information from patients on how their pain has usually been over the past week, even though pain may be reported to vary over the course of a day or from day to day. The HAQ pain scale consists of a doubly anchored, horizontal VAS, that is scored from zero (no pain) to three (severe pain), or alternatively from 0 (no pain) to 100 (severe pain). The VAS for pain has been used widely in experimental, observational, and clinical settings [ 7 – 12 ].
Other Dimensions of the Full HAQ. Drug toxicity data collected by the full HAQ include the drug, dosage, time on drug, specific side effects, degree of severity, the importance to the patient, and subsequent drug course, i.e., whether or not the drug was discontinued due to the side effect. HAQ-derived drug side effect data has permitted the development of a summary Toxicity Index (TI) that quantifies the magnitude of adverse effects (toxicity) associated with specific medications [ 11 , 13 , 14 ]. The TI is a first attempt to quantitatively describe the overall toxicity of medication. Prior adverse effect assessments had used variables comprised of the percentage of patients discontinuing the drug because of side effects or had presented comparative frequencies of selected individual side effects.
Direct cost data that include physician visits, hospital days, laboratory costs, x-rays, medications, and other medical costs including use of alternative treatments and procedures, and indirect cost data due to loss of productivity are captured by the full HAQ.
Death, while obviously not a self-report outcome on the HAQ, is a requisite part of the conceptual model of patient outcome. In this HAQ dimension, mortality-related data, causes, and date of death, are obtained via search of the United States National Death Index.
Both the 2-page and full HAQ contain the HAQ VAS patient global health status scale. It is among the common VAS instruments, which include the Torrance "feeling thermometer" in the EuroQol instrument and the VAS in the Arthritis Impact Measurement Scales, both of which are used to measure quality of life. The HAQ global health status scale is a 15 cm doubly-anchored horizontal VAS that is scored from zero (very well) to 100 (very poor) and has been validated as a measure of quality of life. Fries and Ramey [ 15 ] compared the HAQ global to the Torrance quality-of-life "feeling thermometer" and found the two scales to be highly correlated (r = -0.676; p < 0.001), indicating that both instruments are measuring similar quality of life constructs.
How was the HAQ developed?
The Health Assessment Questionnaire (HAQ) was originally developed in 1978 by James F. Fries, MD, and colleagues at Stanford University. The HAQ Disability Index (HAQ-DI), the original HAQ section to be developed and validated, was initially developed under the auspices of the Stanford Arthritis Center. It recognized the importance of the original American Rheumatism Association functional class measure [ 16 ] and also the lack of sensitivity to change of that four-category measure. The HAQ-DI was developed by parsing questions and components from a variety of instruments extant at the time, and evolved over numerous iterations through a series of subjective and objective assessments via statistical evaluation, physician appraisal, and patient feedback [ 17 ].
The components of the 2-page HAQ (the HAQ-DI, pain scale, and global health status scale) have retained their original content and format since the early 1980s, while the remaining dimensions in the full HAQ are periodically tailored and supplemented with additional questions when contemporary issues arise for specific hypotheses or research questions by ARAMIS or other investigators.
How was the HAQ validated?
The disability index of the HAQ (HAQ-DI) has been validated in numerous studies and disciplines. It has been shown repeatedly to possess face and content validity via comparison with other instruments in multiple disease conditions. The construct/convergent validity, predictive validity, and sensitivity to change have also been established in numerous observational studies and clinical trials. The HAQ-DI has also demonstrated a high level of convergent validity based on the pattern of correlations with other clinical and laboratory measures [ 2 , 11 , 17 – 19 ]. Validity of the HAQ pain scale and the global health status scale have also been demonstrated in numerous studies [ 2 , 11 ].
In which populations has the HAQ been used?
The full HAQ has been deployed in studies with HIV/AIDS patients, normal aging populations, adults and children with rheumatic diseases, and in disabled workers[ 2 , 20 – 22 ]. It has been employed in population-based studies, including the follow-up to the National Health and Nutrition Examination Survey (NHANES) [ 23 ]. It has also been applied to a variety of diseases and conditions, including osteoarthritis, juvenile rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis, fibromyalgia, psoriatic arthritis, systemic sclerosis and has been adapted in many languages for adults as well as children [ 2 ].
What translations are available?
The HAQ Disability Index (HAQ-DI) was originally developed and validated for English-speaking populations in the United States and Canada. It has since been translated or culturally adapted into more than 60 different languages or dialects, often with only minor changes. Table 1 presents a resource listing of translations since 2002. Translations and cultural adaptations of the HAQ-DI are usually carried out by administering investigators. Many have also been performed by the MAPI Research Institute in Lyon, France, and the Health Outcomes Group in Palo Alto, California, both of which have had extensive experience in translating and culturally validating the HAQ-DI; fees are sometimes charged by these vendors.
Translated HAQ-DIs have generally been fully validated, using methods such as test-retest reliability, item-total correlations, convergent validity, interviewer vs. self-administered formats, and factor analyses. Translations are subsequently back-translated by a different translator, and the two English versions compared. This process is repeated until coherence is achieved. To date, culturally adapted HAQ-DI instruments have proved as equally reliable and valid as their parent. To adapt the HAQ-DI culturally, modifications of individual items have sometimes been necessary. The types of items most frequently in need of adaptation have included colloquial expressions or those for which names or types of items or utensils are culturally idiosyncratic. For example, some Asian cultures do not consume milk in cartons; thus, an appropriate substitution in keeping with the original intent of the item is made. In some European countries a bathtub is much more commonly used than is a shower, requiring question modification.
How is the HAQ administered and how long does it take?
The HAQ is usually self-administered, but can also be given face-to-face in a clinical setting or in a telephone interview format by trained outcome assessors, and has been validated in all of these settings. The questionnaire is typically mailed to patients every six months, who are asked to complete it without additional instructions. Patients usually find that the 2-page HAQ is entirely self-explanatory, and clarifications are seldom required. Follow-up phone calls are sometimes needed to obtain missing data or to clarify ambiguous responses in the high-quality research data applications. The HAQ disability index and pain scale can be completed in approximately five minutes. The full HAQ takes 20 to 30 minutes to complete.
How is the HAQ Disability Index (HAQ-DI) and pain scale scored?
The HAQ-DI indicates the extent of the respondent's functional ability, is sensitive to change, and is a good predictor of future disability and costs. It assesses a patient's usual abilities using their usual equipment during the past week. Scoring of the HAQ-DI is patterned after the American Rheumatism Association/American College of Rheumatology functional classes [ 16 , 24 ]. For each item, there is a four-level difficulty scale that is scored from 0 to 3, representing normal (no difficulty) (0), some difficulty (1), much difficulty (2), and unable to do (3). There are 20 questions in eight categories of functioning – dressing, rising, eating, walking, hygiene, reach, grip, and usual activities. The highest component score in each category determines the score for the category, unless aids or devices are required. Dependence on equipment or physical assistance increases a lower score to the level of 2 to more accurately represent underlying disability. A complementary scoring method ignores scores for aids and devices when computing the category scores and represents residual disability after compensatory efforts. The eight category scores are averaged into an overall HAQ-DI score on a scale from zero (no disability) to three (completely disabled). The scale is not truly continuous but has 25 possible values (i.e., 0, 0.125, 0.250, 0.375 … 3). The HAQ-DI score is not computed when the patient provides answers in fewer than six categories. When the HAQ-DI is used to assess disability in a specific disease or condition, usually a single word change can be made in the stem to identify the condition [ 25 , 26 ], which does not change scoring. Disability as measured by the HAQ-DI repeatedly has been correlated with mortality rates, progression of aging, and health care resource utilization [25, 57, 135, 181]. For additional information regarding scoring and analysis, please refer to to the ARAMIS website, http://aramis.stanford.edu , and Bruce B and Fries JF, The Stanford Health Assessment Questionnaire (HAQ): A Review of Its History, Issues, Progress, and Documentation. J Rheumatol. 2003;30(1):167–78.
The HAQ pain scale is designed to obtain data relative to the presence or absence of arthritis-related pain and its severity. The objective is to obtain information from patients on how their pain has usually been over the past week, even though pain may be reported to vary over the course of a day or from day to day. Complete scoring directions are available at the ARAMIS website, http://aramis.stanford.edu .

How are the HAQ-DI scores interpreted?
Scores of 0 to 1 are generally considered to represent mild to moderate difficulty, 1 to 2 moderate to severe disability, and 2 to 3 severe to very severe disability. Average scores that have been reported in a population-based study are 0.49, and in osteoarthritis and rheumatoid arthritis patients are 0.8 and 1.2, respectively. For additional references regarding score interpretation, please see Bruce B and Fries JF, The Stanford Health Assessment Questionnaire (HAQ): A Review of Its History, Issues, Progress, and Documentation. J Rheumatol. 2003;30(1):167–78.
Is the HAQ-DI responsive to change? What is a meaningful change for the HAQ-DI score?
The HAQ-DI is very responsive to change, and usually is the most sensitive to change of the available outcome measures. It is used in the overwhelming majority of studies of rheumatoid arthritis and recommended by the United States Food and Drug Administration and the American College of Rheumatology. Some investigators have suggested that the Minimal Clinical Important Difference is 0.22; others have maintained that 0.10 or thereabouts is clinically important. Additional references may be found in Bruce and Fries, The Stanford Health Assessment Questionnaire (HAQ): A Review of Its History, Issues, Progress, and Documentation. J Rheumatol. 2003;30(1):167–78.
What is the availability and cost of using the HAQ?
The HAQ is copyrighted by Stanford University for the purpose of insuring that it will be used unmodified to preserve the validity of its results and contribute to standardization of assessment across studies. However, it is considered to be in the public domain, with the request that users cite relevant HAQ articles(s) in their publications. There is no charge from Stanford for permission to use the English version of the HAQ. However, other groups that have independently translated the HAQ may charge for their versions.
Who may I contact (Email, fax and phone) to obtain a copy of HAQ?
Judy Rechsteiner, Administrative Assistant
E-mail: [email protected]
Fax: 650/723-9656
Phone: 650/725-4612
How can we obtain more information about the HAQ?
Please go to the ARAMIS website at http://aramis.stanford.edu .
Conclusions
Collection of longitudinal patient outcome data, based on the five patient-centered dimensions, is increasingly standard in clinical trials, epidemiologic studies, and in patient care, representing a major paradigm shift over the past two decades. The HAQ has increased the credibility and use of comprehensive measurement techniques involving validated patient self-report and has led to a new appreciation of outcome assessment. Outcome measurement is rapidly increasing in use, and we anticipate increased focus on a smaller number of instruments with supplemental questions used for disease or study-specific queries. We believe the HAQ to have appropriate attributes to be among those considered for use as standard instruments.
Acknowledgements
Some content and Table 1 adapted from and Bruce B and Fries JF [ 2 ] and are used with permission from the Journal of Rheumatology.
Felson DT, Anderson JJ, Boers M, Bombardier C, Chernoff M, Fried B, Furst D, Goldsmith C, Kieszak S, Lightfoot R, et al .: The American College of Rheumatology preliminary core set of disease activity measures for rheumatoid arthritis clinical trials. The Committee on Outcome Measures in Rheumatoid Arthritis Clinical Trials. Arthritis Rheum 1993, 36 (6):729–40.
Article CAS PubMed Google Scholar
Bruce B, Fries JF: The Stanford health assessment questionnaire (HAQ): a review of its history, issues, progress, and documentation. J Rheumatol 2003, 30 (1):167–78.
PubMed Google Scholar
Fries JF, Ramey DR: Platonic outcomes. J Rheumatol 1993, 20 (3):415–7.
CAS PubMed Google Scholar
Fries J, Spitz P: The hierarchy of patient outcomes. Quality of life assessment for clinical trials (Edited by: Spilker B). New York, Raven press 1990.
Google Scholar
Lorig KR, Cox T, Cuevas Y, Kraines RG, Britton MC: Converging and diverging beliefs about arthritis: Caucasian patients, Spanish speaking patients, and physicians. J Rheumatol 1984, 11 (1):76–9.
Potts M, Mazzuca S, Brandt K: Views of patients and physicians regarding the importance of various aspects of arthritis treatment correlations with health status and patient satisfaction. Pat Ed Coun 1986, 8: 125–34.
Article Google Scholar
Berkanovic E, Oster P, Wong WK, Bulpitt K, Clements P, Sterz M, Paulus H: The relationship between socioeconomic status and recently diagnosed rheumatoid arthritis. Arthritis Care Res 1996, 9 (6):257–62.
Jansen LM, van Schaardenburg D, van Der Horst-Bruinsma IE, Bezemer PD, Dijkmans BA: Predictors of functional status in patients with early rheumatoid arthritis. Ann Rheum Dis 2000, 59 (3):223–6. 10.1136/ard.59.3.223
Article CAS PubMed Central PubMed Google Scholar
Kandziora F, Mittlmeier T, Kerschbaumer F: Stage-related surgery for cervical spine instability in rheumatoid arthritis. Eur Spine J 1999, 8 (5):371–81. 10.1007/s005860050190
Nordenskiold U, Grimby G: Assessments of disability in women with rheumatoid arthritis in relation to grip force and pain. Disabil Rehabil 1997, 19 (1):13–9.
Ramey D, Fries J, Singh G: The Health Assessment Questionnaire 1995 – Status and Review. In: B S, ed. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia: Lippincott-Raven Publishers 2 Edition 1995, 227–37.
Tsakonas E, Fitzgerald AA, Fitzcharles MA, Cividino A, Thorne JC, M'Seffar A, Joseph L, Bombardier C, Esdaile JM: Consequences of delayed therapy with second-line agents in rheumatoid arthritis: a 3 year followup on the hydroxychloroquine in early rheumatoid arthritis (HERA) study. J Rheumatol 2000, 27 (3):623–9.
Singh G, Morfeld D, Shi H, Ramey D, Fries J: Effectiveness and toxicity profiles of drug treatment in RA. Arthritis Rheum 1994, 37: S196.
Singh G, Rosen Ramey D: NSAID induced gastrointestinal complications: the ARAMIS perspective – 1997. Arthritis, Rheumatism, and Aging Medical Information System. J Rheumatol Supplement 1998, 51: 8–16.
CAS Google Scholar
Fries JF, Ramey DR: "Arthritis specific" global health analog scales assess "generic" health related quality-of-life in patients with rheumatoid arthritis. J Rheumatol 1997, 24 (9):1697–702.
Steinbrocker O, Trager C, Betterman R: Therapeutic criteria in rheumatoid arthritis. JAMA 1949, 140: 659–62.
Article CAS Google Scholar
Fries JF, Spitz PW, Young DY: The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol 1982, 9 (5):789–93.
Fries JF, Spitz P, Kraines RG, Holman HR: Measurement of patient outcome in arthritis. Arthritis Rheum 1980, 23 (2):137–45.
Ramey DR, Raynauld JP, Fries JF: The health assessment questionnaire 1992: status and review. Arthritis Care Res 1992, 5 (3):119–29.
Lorig K: Development and dissemination of an arthritis patient education course. Fam Com Health 1986, 9 (1):23–32.
Fries JF, Miller SR, Spitz PW, Williams CA, Hubert HB, Bloch DA: Toward an epidemiology of gastropathy associated with nonsteroidal antiinflammatory drug use. Gastroenterology 1989, 96: 647–55.
Lubeck DP, Fries JF: Health status among persons infected with human immunodeficiency virus. A community-based study. Med Care 1993, 31 (3):269–76.
Hubert HB, Bloch DA, Fries JF: Risk factors for physical disability in an aging cohort: the NHANES I Epidemiologic Followup Study. J Rheumatol 1993, 20 (3):480–8.
Hochberg MC, Chang RW, Dwosh I, Lindsey S, Pincus T, Wolfe F: The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheum 1992, 35 (5):498–502.
Gillen M: Injuries from construction falls. Functional limitations and return to work. AAOHN J 1999, 47 (2):65–73.
Barrett EM, Scott DG, Wiles NJ, Symmons DP: The impact of rheumatoid arthritis on employment status in the early years of disease: a UK community-based study. Rheumatology (Oxford) 2000, 39 (12):1403–9. 10.1093/rheumatology/39.12.1403
Download references
Author information
Authors and affiliations.
School of Medicine, Division of Immunology & Rheumatology Stanford University, USA
Bonnie Bruce & James F Fries
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Bonnie Bruce .
Electronic supplementary material
Additional file 1: (pdf 79 kb), rights and permissions.
Reprints and permissions
About this article
Cite this article.
Bruce, B., Fries, J.F. The Stanford Health Assessment Questionnaire: Dimensions and Practical Applications. Health Qual Life Outcomes 1 , 20 (2003). https://doi.org/10.1186/1477-7525-1-20
Download citation
Received : 09 May 2003
Accepted : 09 June 2003
Published : 09 June 2003
DOI : https://doi.org/10.1186/1477-7525-1-20
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Disability Index
- Stanford Health Assessment Questionnaire
Health and Quality of Life Outcomes
ISSN: 1477-7525
- Submission enquiries: [email protected]
Completing a Health Assessment in Nursing

NurseJournal.org is committed to delivering content that is objective and actionable. To that end, we have built a network of industry professionals across higher education to review our content and ensure we are providing the most helpful information to our readers.
Drawing on their firsthand industry expertise, our Integrity Network members serve as an additional step in our editing process, helping us confirm our content is accurate and up to date. These contributors:
- Suggest changes to inaccurate or misleading information.
- Provide specific, corrective feedback.
- Identify critical information that writers may have missed.
Integrity Network members typically work full time in their industry profession and review content for NurseJournal.org as a side project. All Integrity Network members are paid members of the Red Ventures Education Integrity Network.
Explore our full list of Integrity Network members.
- What is a Comprehensive Health Assessment?
- Beginning an Assessment
Conducting the Physical Exam
Are you ready to earn your online nursing degree.

It’s a common occurrence in any health facility: nurses walk into a room and make a head-to-toe assessment of the patient. This is a critical part of creating a healthcare plan, but what does a nursing health assessment actually entail?
Keep reading to learn more about health assessments in nursing and why they matter.
What is a Comprehensive Health Assessment in Nursing?
Nurses conduct health assessments in clinics, physician offices, hospitals, and emergency rooms. How a nurse performs an assessment depends on the case, namely the person’s age and condition.
All nursing health assessments include paperwork and physical exams. Nurses systematically work on the patient from head to toe, beginning with the least invasive procedure.
Health assessments in nursing begin the moment a nurse walks into the room. Nurses note nonsocial cues. They use their sight and smell to look for symptoms. From there, nurses take a patient’s vital signs — temperature, heart rate, and blood pressure.
Advanced practical nurses (APRNs) may conduct an annual physical exam, while registered nurses (RNs) complete problem-focused exams for patients admitted into hospitals or urgent care departments.
Nursing health assessments help health professionals diagnose diseases and illnesses. Assessments also inform preventative care plans. Through nursing health assessments, nurses can provide guidance and gain patient trust.
Beginning a Nursing Health Assessment
Nursing programs teach students how to conduct nursing health assessments, but nurses often fine tune their skills on the job. Each nurse develops their own style to build patient relationships.
1 Build Patient Rapport
Patients often face social, emotional, and/or cultural barriers in accessing healthcare. Nurses have the power to calm patients — especially from historically excluded communities — who feel anxious or worried about their health.
A nurse’s mannerisms and the questions a nurse asks can build trust. For instance, when nurses start an assessment, they can develop a relationship through an introduction and by explaining what they are about to do. At this point, nurses can also assess a patient’s preference for the physical exam and make an effort to address any fears.
2 Family and Past Health History
On an initial patient visit, nurses ask about family and past medical histories. This information can help shape nursing care plans. During this process, nurses learn of any chronic illnesses, past surgeries, medications taken, sexual activity, and social habits such as smoking or drug use.
During this process, nurses can put patients at ease and build rapport by showing empathy and allowing patients to answer in their own time.
3 General Status and Vital Signs
After a nurse records a patient’s health history, they move to the physical exam. The first part of the physical exam entails the general status check-up. Nurses take vital signs, checking a patient’s heart rate, blood pressure, temperature, and respiratory rate.
Nurses can assess a patient at first sight by taking into account the patient’s posture, emotional state, speech, and hygiene. After nurses take a patient’s vital signs, the physical exam begins. Nurses examine the patient methodically from head to toe, beginning with the head, ears, eyes, nose, and throat (HEENT).
Palpating the head and scalp to check the shape, size, and symmetry can provide information about underlying issues or trauma such as concussions. Nurses also examine facial expressions for drooping or asymmetry, which can help in the diagnosis of a stroke or other conditions that cause facial paralysis. The head assessment also includes:
- Moving hair in sections to look for injuries
- Observing the scalp to look for lice, dandruff, or lesions
- Inspecting the head for masses or tenderness
- Checking that facial movements are symmetrical by asking patients to move their eyebrows or smile
Inspecting the ears using an otoscope can provide insight on hearing loss, vertigo, or tinnitus. Nurses can also identify any cancers or lesions on the outer ear. Ear assessments may also involve:
- Using an otoscope to look for discharge or skin discoloration
- Hitting a tuning fork to test for hearing loss
- Investigating cerumen (earwax) impaction as a cause of hearing loss
- Asking patients about any medications they take
- Checking the inner ear for perforations or swelling in the membrane
Testing the eyes can provide information about a patients’ brain function. A pupil examination can offer signs about head injury. Nurse uses an ophthalmoscope to inspect the external eye functionality. They also:
- Visually inspect the eyes for excessive discharge, redness, or growths
- Record eyesight aids patient uses, including contacts or eyeglasses
- Check the pupils for PERRLA — Pupils: Equal, Round, Reactive to Light, and Accommodation (transitioning focus between close and far objects)
A nose assessment begins by inspecting the exterior for discoloration, symmetry, swelling, malformations, or lesions. For instance, a nurse may note if they find a lesion or dark spot. Using a penlight or the light from an otoscope, nurses examine the nasal cavities for discoloration, discharge, and symmetry. They may continue assessing the nose by:
- Using their thumb to palpate one sinus at a time to identify pain or tenderness
- Closing one nostril at a time to check for normal airflow
- Checking to make sure that the nose is the same color as the patient’s face
A throat inspection can lead to early detection of oral cancer and potentially save someone’s life. Assessments can also help nurses detect strep throat or dysphagia.
Nurses inspect the throat for abnormalities. Throat examinations involve checking the teeth and gums, tongue, uvula, and tonsils, inner lining of the lips and cheeks, and the soft and hard palates. Nurses also:
- Use a tongue depressor to inspect the cheeks for abnormalities such as lesions
- Examine the top and underside of the tongue for discoloration
- Visually inspect the lips for lesions
- Check the coloration of the lips and gums
- Note fouls smells or a fruity scent that could be a sign of ketoacidosis
Nurses inspect the neck to check for jugular venous distention, range of motion, and to see if patients can easily shrug with resistance. A neck examination begins with nurses looking at the location of the trachea to make sure it’s center, and then includes:
- Palpating the sides of the neck to check for swollen lymph nodes
- Checking the neck for tenderness and lumps
- Inspecting thyroid size and shape
- Examining the back of the neck for signs of spinal column injuries
- Looking at the neck for lesions and lumps
Respiratory
Nurses need to know the basics of the respiratory system to recognize signs of respiratory deterioration. Checking the lungs for tenderness and masses, and listening to the lung sounds can provide clues about underlying health issues. Respiratory assessments also include:
- Making visual assessments of a patient’s respiratory rate
- Asking patients if they experience shortness of breath or have a cough
- Placing their hand to the patient’s back to evaluate symmetrical chest rise.
- Using the stethoscope to listen for full inspiration and expiration
- Inspecting the size, shape, and symmetry of the chest
It takes a stethoscope and keen observation skills to perform a cardiac assessment, which provides crucial data about cardiovascular system function. Nurses use palpation and visual cues to look for the quality of cardiac blood flow. The exam often includes:
- Using a stethoscope to auscultate the five points of the heart: Erb’s point and the aortic, pulmonic, tricuspid, and mitral valves
- Palpating the chest wall, looking for vibratory sensations
- Listening for normal heart rates and rhythms
From a supine position, nurses can begin an abdomen examination. This includes auscultation, percussion, and palpation. Nurses may perform abdomen assessments on patients with percutaneous endoscopic gastrostomy feeding tubes or with ostomy pouches. Otherwise routine abdomen assessments include:
- Asking questions about any pain in bowel and urination movements
- Inspecting the abdomen to look at contours and pulsations
- Looking for masses or wounds
- Using the stethoscope to listen to bowel sounds at all four quadrants
- Listening to vascular sounds using the stethoscope’s bell
Pulse assessments tell nurses about a patient’s health status. Nurses look for pulses in different areas of the body — the neck, arms, legs, and feet — depending on the case. During CPR, nurses may check the carotid artery for a pulse to determine if the brain and head are receiving blood flow. Where a nurse looks for a pulse also depends on the patient’s age. Nurses can:
- Check the temporal artery for a pulse
- Find the apical pulse point
- Assess the blood pressure by checking the brachial artery
- Palpate the radial, femoral, posterior tibial, and dorsalis pedi pulse points
Extremities
An essential part of the head-to-toe includes examining the extremities: the arms, hands, legs, and feet. Nurses look for lesions, redness, swelling, injuries, and — in the case of hospitalized patients — they may check the entrypoint of an intravenous line.
A proper assessment can help doctors diagnose gout, diabetes, or deep vein thrombosis. Nurses during an assessment may:
- Palpate the radial artery and joints — the elbows, wrists, and hands — to check skin temperature
- Ask the patient to move and flex their arms and legs against resistance
- Check the color of the legs and toes
- Test extremities for a range of motion
- Inspect the strength and musculature of extremities
Neurological
An examination of coordination, balance, and sensory response can provide information about neurological trauma and prevent long-term damage. In the emergency room and hospital neuro units, patients receive neurological assessments. Nurses also perform neuro exams in other departments. The exams include:
- Using the Romberg test to assess balance
- Checking the gait, including posture
- Examining olfactory and optic nerves
- Checking a patient’s level of consciousness by using the Glasgow Coma Scale
- Assessing orientation and memory by asking a patient routine questions
Frequently Asked Questions About Health Assessments
What is a complete health assessment.
A complete nursing health assessment requires a health professional to examine a patient in a systematic fashion, from head to toe. Nurses rely on self-reported symptoms, visual observation, reported health histories, and a physical medical examination to make a health assessment. This data then informs the nursing care plan.
When are health assessments performed in nursing?
A nursing health assessment helps nurses and other health professionals in a variety of settings to understand a patient’s mental and physical health. In the emergency room, a patient may receive a neurological assessment to test their level of consciousness.
Patients also receive health assessments during their annual physical checkups. At outpatient clinics or long-term care facilities, nurses use health assessments to identify trauma or injury, or to treat disease and illnesses.
Why are nursing health assessments important?
A proper nursing health assessment can lead to early intervention, which saves lives. Nurses also use health assessments to start conversations about social or cultural barriers that patients face in assessing healthcare.
A verbal and physical nursing health assessment helps nurses to gather information about a person’s symptoms, pain, and mobility level. A problem-focused assessment can also direct analysis to specific areas: cardiac, extremities, respiratory, or throat.
What are the four techniques used in physical nursing assessments?
Nurses have a set of skills and tools that they rely on to conduct a nursing health assessment. Health assessments include observation and inspection, palpation, percussion, and auscultation. Nurses perform these techniques sequentially, except during abdominal assessments.
Related Pages

Nursing Diagnosis Guide
How do I use the nursing process and nursing diagnosis in my practice? In this guide, you will learn what is a nursing diagnosis, how to write and use a nursing diagnosis, and the difference between a nursing and medical diagnosis.

The Value of Critical Thinking in Nursing
Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation. Nicholas McGowan, BSN, …

Cultural Competence in Nursing
Cultural competency is a vital skill for delivering quality nursing care across culturally diverse groups. Our guide offers tips from nursing professionals on incorporating it into nursing culture and practice.
Whether you’re looking to get your pre-licensure degree or taking the next step in your career, the education you need could be more affordable than you think. Find the right nursing program for you.
You might be interested in

HESI vs. TEAS Exam: The Differences Explained
Nursing schools use entrance exams to make admissions decisions. Learn about the differences between the HESI vs. TEAS exams.

10 Nursing Schools That Don’t Require TEAS or HESI Exam

For Chiefs’ RB Clyde Edwards-Helaire, Nursing Runs in the Family
Psychological assessment.
- Reference work entry
- First Online: 01 January 2022
- pp 4023–4030
- Cite this reference work entry
- Sofia von Humboldt 3 ,
- Joana Rolo 4 &
- Isabel Leal 3
258 Accesses
Psychodiagnostic assessment ; Psychological battery ; Psychological evaluation ; Psychological testing
Psychological assessment is a testing method that uses a number of techniques to find hypotheses about individuals and their behavior, abilities, and personality (Framingham 2016 ). Psychological testing or psychological assessment is also referred to as conducting a battery of psychological tests on subjects. For different researchers, psychological assessment is a process, in which a psychologist aims: to achieve an accurate description of an individual’s functioning; to identify the person’s clinical needs (e.g., which interventions are more suitable); to make a differential diagnosis of mental disorders of all sorts; and to keep track of the progress made when an intervention is taking place (Meyer et al. 2001 ). A rigorous psychological assessment implies that health professionals also carry out a complete medical examination, to exclude the possibility of a...
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders. Author, Washington, DC
Amieva H, Mokri H, Le Goff M et al (2014) Compensatory mechanisms in higher-educated subjects with Alzheimer’s disease: a study of 20 years of cognitive decline. Brain 137:1167–1175. https://doi.org/10.1093/brain/awu035
Arean PA, Alvidrez J, Barrera A et al (2002) Would older medical patients use psychological services? Gerontologist 42:392–398. https://doi.org/10.1093/geront/42.3.392
Australian Institute of Health and Welfare [AIHW] (2002) Australia’s health 2002. Australian Institute of Health and Welfare, Canberra
Australian Institute of Health and Welfare [AIHW] (2013) Australian hospital statistics 2011–12. Australian Institute of Health and Welfare, Canberra
Bartels SJ, Blow FC, Brockmann LM, Van Citters AD (2005) Substance abuse and mental health care among older Americans: the state of the knowledge and future directions. WESTAT, Rockville
Bertera EM, Bertera RL (2008) Fear of falling and activity avoidance in a national sample of older adults in the United States. Health Soc Work 33:54–62. https://doi.org/10.1093/hsw/33.1.54
Carr D, Luth EA (2017) Advance care planning: contemporary issues and future directions. Innov Aging 1. https://doi.org/10.1093/geroni/igx012
Depp CA, Loughran C, Vahia I, Molinari V (2010) Assessing psychosis in acute and chronic mentally ill older adults. In: Lichtenberg PA (ed) Handbook of assessment in clinical gerontology, 2nd edn. Elsevier, New York, pp 123–154
Edelstein BA, Woodhead EL, Segal DL et al (2007) Older adult psychological assessment: current instrument status and related considerations. Clin Gerontol 31:1–35. https://doi.org/10.1080/07317110802072108
Edelstein BA, Drozdick LW, Ciliberti CM (2010) Assessment of depression and bereavement in older adults. In: Lichtenberg PA (ed) Handbook of assessment in clinical gerontology, 2nd edn. Elsevier, New York, pp 123–154
Framingham J (2016) What is psychological assessment? Psych Cent. https://psychcentral.com/lib/what-is-psychological-assessment/ . Accessed 16 Oct 2018
Gatz M, Smyer M (2001) Mental health and aging at the outset of the twenty-first century. In: Birren JE, Schaie KW (eds) Handbook of the psychology of aging, 5th edn. Academic Press, San Diego, pp 523–544
Gatz M, Smyer MA, DiGilio DA (2016) Psychology’s contribution to the well-being of older Americans. Am Psychol 71:257–267. https://doi.org/10.1037/a0040251
Karel MJ, Gatz M, Smyer MA (2012) Aging and mental health in the decade ahead: what psychologists need to know. Am Psychol 67:184–198. https://doi.org/10.1037/a0025393
Knight BG, Pachana NA (2015) Psychological assessment and therapy with older adults. Oxford University Press, Oxford
Koh S, Blank K, Cohen CI et al (2010) Public’s view of mental health services for the elderly: responses to dear Abby. Psychiatr Serv 61:1146–1149. https://doi.org/10.1176/ps.2010.61.11.1146
Kollack-Walker S, Liu CY, Fleisher AS (2017) The role of neuroimaging in the assessment of the cognitively impaired elderly. Neurol Clin 35:231–262. https://doi.org/10.1016/j.ncl.2017.01.010
La Rue A, Watson J (1998) Psychological assessment of older adults. Prof Psychol Res Pract 29:5–14. https://doi.org/10.1037/0735-7028.29.1.5
Landry GJ, Best JR, Liu-Ambrose T (2015) Measuring sleep quality in older adults: a comparison using subjective and objective methods. Front Aging Neurosci 7:1–10. https://doi.org/10.3389/fnagi.2015.00166
Lawton EM, Shields AJ, Oltmanns TF (2011) Five-factor model personality disorder prototypes in a community sample: self- and informant-reports predicting interview-based dsm diagnoses. Personal Disord Theory Res Treat 2:279–292. https://doi.org/10.1037/a0022617
Maruish ME (2013) Outcomes assessment in health settings. In: Geisinger KF (ed) APA handbook of testing and assessment in psychology, Testing and assessment in clinical and counseling psychology, vol 2. American Psychological Association, Washington, DC, pp 303–324
Mattar S, Khan F (2017) Personality disorders in older adults: diagnosis and management. Prog Neurol Psychiatry 21:22–27. https://doi.org/10.1002/pnp.467
McVay JC, Kane MJ, Kwapil TR (2009) Tracking the train of thought from the laboratory into everyday life: an experience-sampling study of mind wandering across controlled and ecological contexts. Psychon Bull Rev 16:857–863. https://doi.org/10.3758/PBR.16.5.857
Meeks S, Van Haitsma K, Schoenbachler B, Looney SW (2015) BE-ACTIV for depression in nursing homes: primary outcomes of a randomized clinical trial. J Gerontol Ser B 70:13–23. https://doi.org/10.1093/geronb/gbu026
Meyer GJ, Finn SE, Eyde LD et al (2001) Psychological testing and psychological assessment. A review of evidence and issues. Am Psychol 56:128–165. https://doi.org/10.1037//OOO3-O66X.56.2.128
Moore RC, Depp CA, Wetherell JL, Lenze EJ (2016) Ecological momentary assessment versus standard assessment instruments for measuring mindfulness, depressed mood, and anxiety among older adults. J Psychiatr Res 75:116–123. https://doi.org/10.1016/j.jpsychires.2016.01.011
Neikrug AB, Ancoli-Israel S (2010) Sleep disorders in the older adult – a mini-review. Gerontology 56:181–189. https://doi.org/10.1159/000236900
Pryor R (2012) Contemporary issues in the use of psychological assessment for recruitment and selection. InPsych 34:10–13
Qualls SH, Segal DL, Norman S et al (2002) Psychologists in practice with older adults: current patterns, sources of training, and need for continuing education. Prof Psychol Res Pract 33:435–442. https://doi.org/10.1037/0735-7028.33.5.435
Ramsey AT, Wetherell JL, Depp C et al (2016) Feasibility and acceptability of smartphone assessment in older adults with cognitive and emotional difficulties. J Technol Hum Serv 34:209–223. https://doi.org/10.1080/15228835.2016.1170649
Rossi G, Van Den Broeck J, Dierckx E et al (2014) Personality assessment among older adults: the value of personality questionnaires unraveled. Aging Ment Health 18:936–940. https://doi.org/10.1080/13607863.2014.924089
Rossi G, Videler A, van Alphen SPJ (2018) Challenges and developments in the assessment of (mal)adaptive personality and pathological states in older adults. Assessment 25:279–284. https://doi.org/10.1177/1073191116685810
Skelton F, Kunik ME, Regev T, Naik AD (2010) Determining if an older adult can make and execute decisions to live safely at home: a capacity assessment and intervention model. Arch Gerontol Geriatr 50:300–305. https://doi.org/10.1016/j.archger.2009.04.016
Spangenberg L, Forkmann T, Brahler E, Glaesmer H (2011) The association of depression and multimorbidity in the elderly: implications for the assessment of depression. Psychogeriatrics 11:227–234. https://doi.org/10.1111/j.1479-8301.2011.00375.x
Vacha-Haase T (2013) Psychological assessment with older adults. In: APA handbook of testing and assessment in psychology, vol. 2: testing and assessment in clinical and counseling psychology. American Psychological Association, Washington, DC, pp 555–568
Wahl H, Schnabel E (2019) Geropsychology. In: Gu D, Dupre DM (eds) Encyclopedia of gerontology and population aging. Springer, Singapore
Willis TA, Yearall SM, Gregory AM (2011) Self-reported sleep quality and cognitive style in older adults. Cogn Ther Res 35:1–10. https://doi.org/10.1007/s10608-009-9270-x
Wolitzky-Taylor KB, Castriotta N, Lenze EJ et al (2010) Anxiety disorders in older adults: a comprehensive review. Depress Anxiety 27:190–211. https://doi.org/10.1002/ijc.28507
World Health Organization (2017) Mental health of older adults. http://www.who.int/mediacentre/factsheets/fs381/en/ . Accessed 19 Jun 2018
William James Center for Research, ISPA – Instituto Universitário, Lisbon, Portugal
Sofia von Humboldt & Isabel Leal
ISPA – Instituto Universitário, Lisbon, Portugal
Correspondence to Sofia von Humboldt .
Editor information
Editors and affiliations.
Population Division, Department of Economics and Social Affairs, United Nations, New York, NY, USA
Department of Population Health Sciences, Department of Sociology, Duke University, Durham, NC, USA
Matthew E. Dupre
Section Editor information
ISPA-Instituto Universitário, William James Center for Research, Lisbon, Portugal
Sofia von Humboldt Ph.D.
Rights and permissions
Copyright information.
© 2021 Springer Nature Switzerland AG
About this entry
Cite this entry.
von Humboldt, S., Rolo, J., Leal, I. (2021). Psychological Assessment. In: Gu, D., Dupre, M.E. (eds) Encyclopedia of Gerontology and Population Aging. Springer, Cham. https://doi.org/10.1007/978-3-030-22009-9_84
DOI : https://doi.org/10.1007/978-3-030-22009-9_84
Published : 24 May 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-22008-2
Online ISBN : 978-3-030-22009-9
eBook Packages : Social Sciences Reference Module Humanities and Social Sciences Reference Module Business, Economics and Social Sciences
Share this entry
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.316(7140); 1998 Apr 25
Health needs assessment
Development and importance of health needs assessment, john wright.
a Bradford Hospitals NHS Trust, Bradford Royal Infirmary, Bradford BD9 6RJ, b Nuffield Institute for Health, Leeds LS2 9PL, c North Yorkshire Health Authority, York YO1 1PE
Rhys Williams
John r wilkinson.
Most doctors are used to assessing the health needs of their individual patients. Through professional training and clinical experience we have developed a systematic approach to this assessment and we use it before we start a treatment that we believe to be effective. Such a systematic approach has often been missing when it comes to assessing the health needs of a local or practice population.

The health needs of individual patients coming through the consulting room door may not reflect the wider health needs of the community. If people have a health problem that they believe cannot be helped by the health service, then they will not attend. For example, many people with angina or multiple sclerosis are not known to either their local general practitioner or to a hospital specialist. 1 , 2 Other groups of patients who may need health care but do not demand it include homeless people and people with chronic mental illness.
Distinguishing between individual needs and the wider needs of the community is important in the planning and provision of local health services. If these needs are ignored then there is a danger of a top-down approach to providing health services, which relies too heavily on what a few people perceive to be the needs of the population rather than what they actually are.
Summary points
- Health needs assessment is the systematic approach to ensuring that the health service uses its resources to improve the health of the population in the most efficient way
- It involves epidemiological, qualitative, and comparative methods to describe health problems of a population; identify inequalities in health and access to services; and determine priorities for the most effective use of resources
- Health needs are those that can benefit from health care or from wider social and environmental changes
- Successful health needs assessments require a practical understanding of what is involved, the time and resources necessary to undertake assessments, and sufficient integration of the results into planning and commissioning of local services
What is health needs assessment?
Health needs assessment is a new phrase to describe the development and refinement of well established approaches to understanding the needs of a local population. In the 19th century the first medical officers for health were responsible for assessing the needs of their local populations. More recently, in the 1970s the Resource Allocation Working Party assessed relative health needs on the basis of standardised mortality ratios and socioeconomic deprivation in different populations, and it used this formula to recommend fairer redistribution of health service resources. 3 The 1992 Health of the Nation initiative was a government attempt to assess national health needs and determine priorities for improving health. 4 Health needs assessment has come to mean an objective and valid method of tailoring health services—an evidence based approach to commissioning and planning health services.
Although health needs assessments have traditionally been undertaken by public health professionals looking at their local population, these local health needs should be paramount to all health professionals. Hospitals and primary care teams should both aim to develop services to match the needs of their local populations. Combining population needs assessment with personal knowledge of patients’ needs may help to meet this goal. 5
Why has needs assessment become important?
The costs of health care are rising. Over the past 30 years expenditure on health care has risen much faster than the cost increases reported in other sectors of the economy, and health care is now one of the largest sectors in most developed countries. 6 Medical advances and demographic changes will continue the upward pressure on costs. 7
At the same time the resources available for health care are limited. Many people have inequitable access to adequate health care, and many governments are unable to provide such care universally. In addition there is a large variation in availability and use of health care by geographical area and point of provision. 8 Availability tends to be inversely related to the need of the population served. 9
Another force for change is consumerism. The expectations of members of the public have led to greater concerns about the quality of the services they receive—from access and equity to appropriateness and effectiveness.
These factors have triggered reforms of health services in both developed and developing countries. In Britain these reforms resulted in the separation of the responsibility for financing health care from its provision and in the establishment of a purchasing role for health authorities and general practitioners. Health authorities had greater opportunities to try to tailor local services to their own populations, and the 1990 National Health Service Act required health authorities to assess health needs of their populations and to use these assessments to set priorities to improve the health of their local population. 10 , 11 This has been reinforced by more recent work on inequalities in health, suggesting that health authorities should undertake “equity audits” to determine if healthcare resources are being used in accordance with need. 12
At a primary care level, through fundholding, locality commissioning, and total purchasing projects, general practitioners have become more central to strategic planning and development of health services. With this increased commissioning power has come the increased expectation from patients and politicians that decision making would reflect local and national priorities, promoting effective and equitable care on the basis of need. 13 The Labour government has committed itself to ensuring access to treatment according to “need and need alone,” and the key functions of primary care groups will be to plan, commission, and monitor local health services to meet identified local needs. 14 , 15
Doctors, sociologists, philosophers, and economists all have different views of what needs are. 16 – 20 In recognition of the scarcity of resources available to meet these needs, health needs are often differentiated as needs, demands, and supply (fig (fig1). 1 ).

Different aspects of needs
in health care is commonly defined as the capacity to benefit. If health needs are to be identified then an effective intervention should be available to meet these needs and improve health. There will be no benefit from an intervention that is not effective or if there are no resources available.
is what patients ask for; it is the needs that most doctors encounter. General practitioners have a key role as gatekeepers in controlling this demand, and waiting lists become a surrogate marker and an influence on this demand. Demand from patients for a service can depend on the characteristics of the patient or on the media’s interest in the service. Demand can also be induced by supply: geographical variation in hospital admission rates is explained more by the supply of hospital beds than by indicators of mortality 21 , 22 ; referral rates of general practitioners owe more to the characteristics of individual doctors than to the health of their populations. 23
is the health care provided. This will depend on the interests of health professionals, the priorities of politicians, and the amount of money available. National health technology assessment programmes have developed in recognition of the importance of assessing the supply of new services and treatments before their widespread introduction.
Need, demand, and supply overlap, and this relation is important to consider when assessing health needs (fig (fig2 2 ). 20

Relation between need, supply, and demand—central area shows ideal relation. Modified from Stevens and Raferty. 24
Health needs
The World Health Organisation’s definition of health is often used: “Health is a state of complete physical, psychological, and social wellbeing and not simply the absence of disease or infirmity.” A more romantic definition would be Freud’s: “Health is the ability to work and to love.”
Healthcare needs
are those that can benefit from health care (health education, disease prevention, diagnosis, treatment, rehabilitation, terminal care). Most doctors will consider needs in terms of healthcare services that they can supply. Patients, however, may have a different view of what would make them healthier—for example, a job, a bus route to the hospital or health centre, or decent housing.
incorporate the wider social and environmental determinants of health, such as deprivation, housing, diet, education, employment. This wider definition allows us to look beyond the confines of the medical model based on health services, to the wider influences on health (box). Health needs of a population will be constantly changing, and many will not be amenable to medical intervention.
Influences on health
- Environment: housing, education, socioeconomic status, pollution
- Behaviour: diet, smoking, exercise
- Genes: inherited health potential
- Health care: including primary, secondary, and tertiary prevention
Assessment of health needs is not simply a process of listening to patients or relying on personal experience. It is a systematic method of identifying unmet health and healthcare needs of a population and making changes to meet these unmet needs. It involves an epidemiological and qualitative approach to determining priorities which incorporates clinical and cost effectiveness and patients’ perspectives. This approach must balance clinical, ethical, and economic considerations of need—that is, what should be done, what can be done, and what can be afforded. 25
Health needs assessment should not just be a method of measuring ill health, as this assumes that something can be done to tackle it. Incorporating the concept of a capacity to benefit introduces the importance of effectiveness of health interventions and attempts to make explicit what benefits are being pursued. Economists argue that the capacity to benefit is always going to be greater than available resources and that health needs assessment should also incorporate questions of priority setting, 26 suggesting that many needs assessments are simply distractions from the difficult decisions of rationing. 27
For individual practices and health professionals, health needs assessment provides the opportunity for:
- Describing the patterns of disease in the local population and the differences from district, regional, or national disease patterns;
- Learning more about the needs and priorities of their patients and the local population;
- Highlighting the areas of unmet need and providing a clear set of objectives to work towards to meet these needs;
- Deciding rationally how to use resources to improve their local population’s health in the most effective and efficient way;
- Influencing policy, interagency collaboration, or research and development priorities.
Importantly, health needs assessment also provides a method of monitoring and promoting equity in the provision and use of health services and addressing inequalities in health. 28 , 29
The importance of assessing health needs rather than reacting to health demands is widely recognised, and there are many examples of needs assessment in primary and secondary care. 21 , 30 , 31
There is no easy, quick-fix recipe for health needs assessment. Different topics will require different approaches. These may involve a combination of qualitative and quantitative research methods to collect original information, or adapting and transferring what is already known or available.
The stimulus for these assessments is often the personal interest of an individual or the availability of new funding for the development of health services. However, assessments should also be prompted by the importance of the health problem (in terms of frequency, impact, or cost), the occurrence of critical incidents (the death of a patient turned away because the intensive care unit is full), evidence of effectiveness of an intervention, or publication of new research findings about the burden of a disease.
Why do projects fail?
Some needs assessments have been more successful than others. Projects may fail for several reasons. 31 – 33
Firstly, what is involved in assessing health needs and how it should be undertaken may not be understood. Educational strategies can improve the understanding and necessary skills of health professionals, and local public health teams can provide valuable support and guidance. Common sense can be a more important asset than detailed methodological understanding. 34 Starting with a simple and well defined health topic can provide experience and encourage success.
Secondly, projects may fail because of a lack of time, resources, or commitment. The time and resources required can be small when shared among professionals in a team, and such sharing has the potential to be team building. Involving other organisations such as social services, local authorities, or voluntary groups can provide similar advantages and encourage multiagency working. Integration of needs assessment into audit and education can also provide better use of scarce time. Such investment of time and effort is likely to become increasingly necessary in order to justify extra resources.
A third reason is the failure to integrate the results with planning and purchasing intentions to ensure change. The planning cycle should begin with the assessment of need. 28 Objectives must be clearly defined (box) and relevant stakeholders or agencies—be they primary care teams, hospital staff, health authorities, the voluntary sector, the media, regional executives, government, or patients—must be involved appropriately (fig (fig3). 3 ). Although such an assessment may produce a multitude of needs, criteria can be used to prioritise these needs—for example, the importance of a problem in terms of frequency or severity, the evidence of effectiveness of interventions, or the feasibility for change. Needs assessments that do not include sufficient attention to implementation will become little more than academic or public relations exercises.
Questions to ask when assessing health needs
- What is the problem?
- What is the size and nature of the problem?
- What are the current services?
- What do patients want?
- What are the most appropriate and effective (clinical and cost) solutions?
- What are the resource implications?
- What are the outcomes to evaluate change and the criteria to audit success?

Contributors to needs assessment
This series will describe the different approaches to assessing health needs, how to identify topics for health needs assessments, which practical approaches can be taken, and how the results can be used effectively to improve the health of local populations. It will give examples of needs assessment from primary care but will also cover the specific problems of needs assessment for hard to reach groups. Many of the techniques of community appraisals used in needs assessment originate from experience in developing countries, and some of the lessons from this experience will be described.
These articles have been adapted from Health Needs Assessment in Practice , edited by John Wright, which will be published in July
Acknowledgments
We are grateful to John Bibby and Dee Kyle for their valuable contributions and to Margaret Haigh for secretarial support.
Funding: None.
Conflict of interest: None.
- Published: 16 May 2024
Multimorbidity prevalence and health outcome prediction: assessing the impact of lookback periods, disease count, and definition criteria in health administrative data at the population-based level
- Marc Simard 1 , 2 , 3 , 4 ,
- Elham Rahme 5 ,
- Marjolaine Dubé 1 ,
- Véronique Boiteau 1 ,
- Denis Talbot 2 , 3 &
- Caroline Sirois 1 , 3 , 4 , 6
BMC Medical Research Methodology volume 24 , Article number: 113 ( 2024 ) Cite this article
Health administrative databases play a crucial role in population-level multimorbidity surveillance. Determining the appropriate retrospective or lookback period (LP) for observing prevalent and newly diagnosed diseases in administrative data presents challenge in estimating multimorbidity prevalence and predicting health outcome. The aim of this population-based study was to assess the impact of LP on multimorbidity prevalence and health outcomes prediction across three multimorbidity definitions, three lists of diseases used for multimorbidity assessment, and six health outcomes.
We conducted a population-based study including all individuals ages > 65 years on April 1st, 2019, in Québec, Canada. We considered three lists of diseases labeled according to the number of chronic conditions it considered: (1) L60 included 60 chronic conditions from the International Classification of Diseases (ICD); (2) L20 included a core of 20 chronic conditions; and (3) L31 included 31 chronic conditions from the Charlson and Elixhauser indices. For each list, we: (1) measured multimorbidity prevalence for three multimorbidity definitions (at least two [MM2+], three [MM3+] or four (MM4+) chronic conditions); and (2) evaluated capacity ( c-statistic ) to predict 1-year outcomes (mortality, hospitalisation, polypharmacy, and general practitioner, specialist, or emergency department visits) using LPs ranging from 1 to 20 years.
Increase in multimorbidity prevalence decelerated after 5–10 years (e.g., MM2+, L31: LP = 1y: 14%, LP = 10y: 58%, LP = 20y: 69%). Within the 5–10 years LP range, predictive performance was better for L20 than L60 (e.g., LP = 7y, mortality, MM3+: L20 [0.798;95%CI:0.797-0.800] vs. L60 [0.779; 95%CI:0.777–0.781]) and typically better for MM3 + and MM4 + definitions (e.g., LP = 7y, mortality, L60: MM4+ [0.788;95%CI:0.786–0.790] vs. MM2+ [0.768;95%CI:0.766–0.770]).
In our databases, ten years of data was required for stable estimation of multimorbidity prevalence. Within that range, the L20 and multimorbidity definitions MM3 + or MM4 + reached maximal predictive performance.
Peer Review reports
Multimorbidity is a complex condition associated with poor health outcomes, polypharmacy, and high healthcare utilisation [ 1 ]. It is particularly prevalent in older adults [≥ 65 years old], with more than half cumulating two or more chronic conditions [ 2 ]. The most common criteria used to define multimorbidity (MM) are based on the count of different chronic conditions [ 3 ], such as at least two (MM2+), three (MM3+) or four (MM4+) chronic diseases. From a public health perspective, multimorbidity measures based on the count of chronic conditions are useful to decision makers who must consider multiple health outcomes simultaneously to plan appropriate interventions [ 4 ]. Moreover, because of their simplicity and ease of interpretation, they are gaining popularity among clinicians and the lay public [ 4 ].
Health administrative databases are extensively used for surveillance and research purposes to measure multimorbidity prevalence at the population level, particularly in single-payer healthcare systems such as those in Australia, Canada, UK, Taiwan and many European countries [ 5 ]. Yet the creation of multimorbidity measures based on the count of chronic conditions entails several methodological choices that can affect their validity and predictive performance. For one, the length of the optimal retrospective period of search for relevant healthcare encounters remains an issue. Health administrative databases comprise a sequential collection of codes for prevalent and newly diagnosed diseases captured in one or many data files during medical visits or hospitalisation stays. Therefore, a minimal retrospective period of search for diagnosis codes (“lookback period” [LP]) is required to accurately capture the chronic conditions of each person registered. A LP that is too short may underestimate the prevalence of multimorbidity, while a LP that is too long may complicate data extraction and increase the probability of erroneously capturing resolved conditions from previous years.
The choice of LP may therefore impact both the prevalence of multimorbidity and its capacity to predict health outcomes; however, these elements have never been jointly assessed. Some studies have assessed the impact of the LP on the prevalence of multimorbidity. Among Danish adults aged 65 and over in 2015, the prevalence of MM2 + increased from 10 to 52% as the LP increased from 1 to 15 years, with a relative stabilization around 10 years [ 6 ]. Higher prevalence with increasing LP was also observed among Canadian patients hospitalized in the early 2000s for cardiovascular diseases [ 7 ] and or HIV [ 8 ]. Other studies have assessed outcome predictions in association with LP. In Canadian patients newly diagnosed with hypertension in the early 2000s, the performance of the MM2 + criterion in predicting 1-year mortality increased when the LP was extended from 6 to 12 months, with c-statistic values increasing from 0.89 to 0.91 [ 9 ]. In a Australian cohort of hospitalized patients between 1990 and 1996, increasing the LP from 1 to 5 years resulted in a small increase in the prediction of 30-day readmission ( c-statistic values increasing from 0.67 to 0.68) but had no impact on 1-year mortality ( c-statistic remaining unchanged at 0.90) [ 10 ]. However, the latter studies had several shortcomings when assessing outcome prediction: (1) maximal LP was limited to 5 years; (2) analyses were conducted in subgroups and not in the general population; (3) some but not all health outcomes considered of interest were evaluated. In addition, no study has previously assessed jointly the prevalence of multimorbidity and its predictive performance according to the LP.
Both the multimorbidity prevalence and the capacity of multimorbidity to predict health outcomes are influenced by two elements: (1) the number of diseases included in the multimorbidity measure, and (2) the criterion used to define multimorbidity (e.g., MM2+, MM3+, MM4+) [ 11 , 12 ]. However, it remains unclear how the LP interact with these two aspects and thus affect multimorbidity prevalence and predictive capacity.
The primary objective of this study was to evaluate the impact of the LP on the prevalence of multimorbidity and the prediction of six health outcomes in the general population among individuals over 65 years of age. The secondary objective was to assess whether variations in the list of diseases included in the multimorbidity measure or the choice of criterion used to define multimorbidity can influence the impact of LP in this population.
Data source and population
Our population-based cohort study included all individuals over the age of 65 registered in the Québec Integrated Chronic Disease Surveillance System (QICDSS) on April 1st, 2019, (cohort entry date) and followed them for one year. The QICDSS links provincial health services administrative data since 1996 using a unique patient identifier [ 13 ]. The data include demographic, death registry, physician claims, and pharmaceutical claims records obtained from the Provincial health insurance board (Régie de l’assurance maladie du Québec [RAMQ]) as well has hospital discharge abstract records (MED-ECHO) owned by the Quebec Ministry of Health and housed at RAMQ. Demographic data includes place of residence, age, sex and neighbourhood-level social and material deprivation quintiles [ 14 ]. Physician claims include diagnoses coded using the International Classification of Diseases, 9th Revision, Quebec adaptation (ICD-9-QC) and the ICD 10th Revision Canadian Coding Standard (ICD-10-CA) since January 1st, 2019. Hospital discharge records include the admission diagnosis, primary diagnosis and up to 29 secondary diagnoses coded using ICD-9-QC system until March 31, 2006, and ICD-10-CA system thereafter. As the province of Quebec has a universal healthcare system, the QICDSS includes medical records for over 99% of the population. In addition, drug insurance is mandatory in Quebec. All individuals aged 65 years and older are eligible for coverage by the public drug plan. However, approximately 10% is not covered due to either their preference to retain their private insurance plan or their medication being provided by the nursing home where they reside.
Multimorbidity measure
We considered three widely used criteria to define multimorbidity: MM2+, MM3+, MM4+ [ 3 ]. We also identified three lists of medical conditions commonly used to build the multimorbidity measures. These lists were deemed representative of the high diversity of medical conditions included in multimorbidity measures relying on health administrative data [ 5 ] (The lists of diseases and ICD codes for each list are available in Supplemental Digital Content [SDC] 01: Tables A1.1 - A1.4 ). First, the “All-inclusive list”(L60) included all ICD codes corresponding to chronic diseases grouped into 60 diseases by a multidisciplinary team [ 15 ]. This list was considered of high quality in a previous systematic review because it met six of the eight quality criteria used to define robust multimorbidity measures methodology [ 5 ]. Second, the “Core list” (L20) included a minimal core of 20 diseases identified in a systematic review by Ho and colleagues [ 3 ]. This minimum core of diseases includes chronic conditions with the highest disability adjusted life-years (DALYs) or years of life lost (YLLs) from the Global Burden of Disease Project [ 16 ]. We added osteoporosis to that list because this chronic condition was reported among the top 20 with the highest impact on DALY in Canada [ 17 ]. Third, the “Charlson & Elixhauser list” (L31) included 31 diseases from the Combined comorbidity index, a combination of both Charlson and Elixhauser comorbidity indices [ 11 , 12 ].
We employed varying LP ranging from 1 to 20 years to estimate multimorbidity prevalence at the cohort entry date (April 1, 2019). We retrospectively retrieved ICD diagnosis codes for each person and medical condition from hospitalization and physician records until April 1st, 1999 (Fig. 1 ). The choice of a 20-year LP was based on the availability of data in QICDSS, limiting our analysis to this timeframe. We used the algorithm proposed by Klabunde et al. [ 18 ] to identify each disease in the administrative databases: we searched both inpatient and outpatient records and identified an individual as having a disease if (1) at least one diagnosis code (primary or secondary) was recorded in the hospitalization records or (2) at least two diagnosis codes were recorded in inpatient or outpatient physician claims within two years and at least 30 days apart.

Illustration of the assessment of multimorbidity prevalence at index date with varied lookback periods (LPs) and 1-year health outcome measurements. For example, for a person aged 66 on April 1 st , 2019, the retrospective search in both inpatient and outpatient databases using a LP of 1 year runs from April 1 st , 2018 to March 31 th , 2019. Using a LP of 20 years, it extends from April 1 st 1999 to March 31 th , 2019
We investigated the capacity of each multimorbidity measure, computed on April 1st, 2019, to predict six health outcomes that have been associated with multimorbidity and were measurable in the QICDSS during the 1-year follow-up (until March 31th, 2020): all-cause mortality, polypharmacy, hospitalisation and frequent visits to the emergency department (ED), to the general practitioner (GP) and to any specialist physician (SP). We defined polypharmacy as ≥ 10 different medications claimed in the follow-up year. We used the common denomination (each active ingredient or combination has a distinct common denomination code) to identify each medication claimed. Those claims included medications for acute and chronic conditions. We defined frequent ED visits using a commonly used threshold of ≥ 3 visits in the follow-up year [ 19 ]. A single visit to the ED was defined as 1 or more ED–related claims on up to 2 consecutive days [ 20 ]. Frequent visits to any GP (≥ 7 visits) or any SP (≥ 10 visits) in the follow-up year were defined using the 95th percentile in the annual number of ED visits in the Québec adult population [ 21 , 22 ].
Statistical analysis
We estimated the prevalence of multimorbidity for each criterion used to define multimorbidity, each list of diseases, and each LP (1 to 20 years) and calculated the relative change in multimorbidity prevalence for each additional year of lookback (Fig. 1 ).
Then, we used logistic regression models to assess the impact of each criterion used to define multimorbidity on the health outcome. We first built one baseline model for each health outcome where the health outcome was the dependent variable and the covariates (age group, sex, material and social deprivations) were predictors. To estimate the performance of the multimorbidity measures in predicting each health outcome over and beyond that of the baseline covariates and to assess the impact of the LP on the prediction performance, we built 1080 logistic regression models for each combination of criterion used to define multimorbidity (3 criteria), list of diseases (3 lists), LP (20 periods) and health outcomes (6 outcomes). Of note, the analysis of polypharmacy and health services outcomes (hospitalisation, ED, GP, SP visits) included only those alive and covered by the drug plan during the entire one-year follow-up. Performance of each model was assessed using three measures: (1) the discrimination capacity of each model, that is the ability to identify correctly patients having the outcome within 1 year, with the c-statistic (also known as the area under the receiver operating characteristic curve) [ 23 ] (A difference in c-statistic superior to [0.010] was considered significant because covariates that contribute such difference may reduce confounding bias in observational studies [ 24 ]); (2) the overall performance of the model calculated with the scaled Brier score, which values range from 0 to 1 (higher value indicates better performance); and (3) the level of agreement between observed and predicted probability of the outcome using calibration intercept and slope, for which a value near zero and one indicates a better prediction, respectively [ 23 ].
All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
Supplementary and sensitivity analyses
Considering the recognized variations in claims history, risk of mortality and healthcare resource utilization associated with age and sex, we conducted stratified analyses to estimate the predictive performance according to these factors. We categorized age groups as 66–79 and ≥ 80 years, and also considered sex as a stratification factor. This approach allowed us to investigate the internal validity by assessing performance heterogeneity between these groups and is preferred to approaches that assess average performances (e.g., via bootstrapping), given the large size of the samples and the low complexity of the models [ 25 ].
We also repeated all the analyses using disease specific algorithms to take into account the shorter period of chronicity of some diseases. Because such algorithms are proposed in the literature only for all diseases included in the “Core list”(L20), we used them only for this list. Those algorithms are described in the supplementary material (SDC01: Table A1.3 ). For the “All-inclusive list”(L60) and the “Charlson & Elixhauser list”(L31), we limited the length of LP to 5 years for all mental health disorders having a remitting or relapsing course in these two lists [ 26 , 27 ]. For the “Core list” (L20), we also re-ran all analyses by adding one supplementary disease (hypertension) to the list as hypertension is included in a majority of multimorbidity measures [ 3 ].
The study population included more than 1.4 million individuals older than 65 years (Table 1 ). The mean age was 75 years and 55% of individuals were female. Death occurred in 4% of the cohort. Other health outcomes were observed in proportions varying between 5% and 38%.
Lookback and prevalence
The prevalence of multimorbidity increased with the length of the LP for each criterion used to define multimorbidity and for each list of diseases (Fig. 2 ). As expected, the prevalence of multimorbidity was higher for the “All-inclusive list”(L60) than for the “Core list”(L20). Using the MM2 + criterion, the multimorbidity prevalence was more than 1.5 times higher in the “All-inclusive list”(L60) (68% [5 years LP]; 84% [10 years LP]) than in the “Core list”(L20) (40% [5 years LP]; 55% [10 years LP]) (Fig. 2 ; SDC: Table A2.1 ). Prevalence estimates of the “Charlson & Elixhauser list”(L31) were quite similar to the “Core list”(L20). For each list of diseases and each criterion used to define multimorbidity, the multimorbidity prevalence increased when LP increased. More precisely, the prevalence increased more rapidly when the lookback period is less than 5 years, while the increase became less pronounced when the lookback period extends beyond 10 years. For example, for the “Core list” (L20), prevalence increased incrementally from 11% to 40%, 55%, 63%, and 69% as the LP increased from 1 to 5, 10, 15, and 20 years (Fig. 2 ; SDC: Table A2.1 ).
Lookback and predictive performance
The length of the LP for which a maximal performance in prediction was reached varied widely (Fig. 3 ). For example, the maximum performance for predicting mortality with the “All-inclusive list”(L60) was achieved with a LP of 2 years compared to 20 years for predicting polypharmacy with the “Core list” (L20). Globally, a shorter length of LP was required for the “All-inclusive list” (L60) than for the “Core list” (L20). In the “All-inclusive list” (L60), the maximal performance was reached with a LP < 5 years for all health outcomes except polypharmacy and frequent visits to the GP (LP = 7 years for both outcomes). In the “Core list” (L20), the maximal performance was reached when the LP varied between 5 and 10 years for all outcomes, except polypharmacy and frequent visits to the GP (LP > 10 years). Nonetheless, the maximum performance values were quite similar for both these two lists (Table 2 ). In both cases, the highest value of the c-statistic was observed with mortality (> 0.800). The performance of the “Charlson & Elixhauser list” (L31) was lower than the two other lists for frequent visits to GP or SP (L60 only), but higher for mortality and polypharmacy.
Prediction performance also varied according to the criterion used to define multimorbidity (Fig. 3 ). The maximum performance was generally observed for MM3 + or MM4+ (Table 2 ). Calibration intercept was close to zero and slope close to one for all models (results not shown).
When the prevalence of multimorbidity stabilized, that is between 5 and 10 years LP, the “Core list” (L20) performed better than the “All-inclusive list” (L60), except for frequent visits to SP (Table 3 , SDC02: Tables A2.2.1 - A2.4.6 ). For example, with a LP of 7 years, the c-statistic value for 1-year mortality prediction was 0.798 for the “Core list” (L20) and 0.788 for the “All-inclusive list” (L60) (Table 3 ). The “Charlson & Elixhauser list” (L31) had similar performance to the “Core list” (L20), but performed better at 1-year mortality prediction.
Supplementary and sensitivity analysis
The impact of the length of LP on predictive performance was homogeneous across lists of diseases among age and sex subpopulations. This indicates that variation in age or sex has low impact on the validity of the predictive models (SDC02: Figures A1.1 , A1.2 ; Tables A3.1 , A3.2 ).
Using a validated case definition for each disease in the “Core list”(L20) had virtually no impact on performance, but it led to a decrease in prevalence. Conversely, adding hypertension to this list had no impact on the performance but increased the prevalence (SDC02: Tables A2.1 , A2.3.1 - A2.3.6 ). Limiting the LP to 5 years for mental disorders had no impact on the main findings for the “Charlson & Elixhauser list”(L31) and the “All-inclusive list”(L60) (SDC02: Tables A2.1 , A2.2.1 - A2.2.6 , A2.4.1 - A2.4.6 ).
In this population-based study, we found that the LP impacted both multimorbidity prevalence estimates and health outcome prediction. As expected, the prevalence of multimorbidity increased with increasing LPs. The increased rate was similar among all lists of diseases and criteria used to define multimorbidity. Our results suggest that multimorbidity increases when LP increases and that underestimation in prevalence appears less pronounced after 10 years of LP. LPs required to achieve optimal performance varied across diseases lists, criteria used to define multimorbidity and health outcomes. Furthermore, the maximal performance was observed almost exclusively for MM3 + or MM4 + regardless of the list of diseases and for all outcomes.
Implication
The threefold impact of LP, list of diseases, and criteria used to define multimorbidity on predictive performance may create potential dilemma if there is a need to both estimate multimorbidity prevalence and predict health outcomes. Indeed, if a LP < 5 years clearly underestimates the prevalence of multimorbidity, peak prediction performance for some list of diseases can be reached within the 1–5 years LP range. Fortunately, the “Core list” (L20) might resolve, at least partially, this dilemma as the maximal predictive performance for most outcomes was reached when the LP was higher than 5 years. Our study underscores that availability of data, and hence the possible LP length, might impact the choice of the list of diseases and/or the selection of criterion used to define multimorbidity. For example, if the database allows only for a short LP (e.g., 2 years), a more inclusive list of diseases or the MM2 + criterion might be worthwhile.
Better performance of MM3 + or MM4 + in predicting health outcomes suggests that in the population aged > 65 years, defining multimorbidity as the co-occurrence of at least 3 or at least 4 diseases would allow for better identification of a sub-populations at higher risk for health outcomes.
Interpretation within the context of the literature
The rapidity with which the multimorbidity prevalence “stabilized” as LP increased was lower in our study than what was observed in a Danish Study with a population of a similar age [ 6 ]. In that study, the MM2 + prevalence increased from 51 to 52% when LP increase from 10 to 15 years compared to 55–63% with the “Core list”[L20]). Nevertheless, results of both the Danish study and ours suggested that at least 5 to 10 years of LP are needed to limit the underestimation of multimorbidity prevalence. A reduction in prevalence underestimation after 10 years of LP was also observed for the eight chronic conditions included in a cohort of HIV patients [ 8 ].
A change in predictive performance with increasing LPs was also observed in other studies [ 9 , 10 ]. Among Canadian patients newly diagnosed with hypertension in the early 2000s, the c-statistic value for prediction of hospitalization increased from 0.756 to 0.768 when the LP increased from 6 to 12 months and then remained similar until the maximum LP of 3 years [ 9 ]. In an Australian cohort of patients hospitalized between 1990 and 1996, the c-statistic value for re-hospitalization prediction increased continuously from 0.640 to 0.656 when the LP increased from 1 to 5 years [ 10 ]. Interestingly, we observed a reduction in predictive performance beyond a certain LP for several outcomes in our study, and the reduction was more pronounced for the list with the largest number of chronic diseases (L60). For example, we observed a reduction of 0.023 in the c-statistic for mortality when LP increased from 2 years ( c-statistic = 0.800) to 20 years ( c-statistic = 0.777) with the L20 list, and 0.032 with the L60 list. These results could imply that, to some extent, diagnosis codes of prevalent and newly diagnosed conditions observed long in the past may have a limited impact on current health outcomes. Maximal predictive performance is reached with very short LP for some outcomes. Such performance might be attributed not only to the count of chronic conditions, but also to recent healthcare resource use. Indeed, short LPs are more likely to capture diagnoses from individuals who frequently utilize healthcare resources.
Strengths and limitations
This is the first study to assess the impact of the LP on both multimorbidity prevalence and health outcome prediction in a general population setting. Selection bias was minimized as the data registry included almost the entire population over age 65 in the province of Québec, Canada. Another strength of the study is that we identified diseases using both outpatient and inpatient data and that we had data on health conditions retrospectively for more than 20 years. The use of either one of these datasets alone (inpatient or outpatient) would have underestimated both the prevalence and predictive performances [ 9 ]. We also included six health outcomes, allowing us to observe that the length of the LP required to maximize the predictive performance varied from 2 to 20 years. We also used a broad representativeness of disease lists used in administrative data. Nonetheless, generalization of our results to other lists used in multimorbidity measures should be made with caution. While multimorbidity measures based on the count of chronic diseases are useful when considering multiple health outcomes simultaneously, measures based on weighted indices like the Charlson Index or the Combined index (a combination of the Charlson and Elixhauser indices) might be more appropriate when focusing on a specific outcome. For instance, Kondalsamy-Chennakesavan et al. developed an adapted version of the Charlson index to predict surgical adverse events [ 28 ]. However, one drawback of such indices is that their weighting requires regular revision, as it can vary over time and depending on the population being studied [ 11 ].
A LP of ten years allowed to limit the underestimation of multimorbidity prevalence in health administrative databases. The optimal predictive performance is often reached when LP is smaller than 10 years according to the outcome or the number of diseases included in the list of diseases. This dilemma of balancing reliable multimorbidity prevalence and optimal outcome prediction complicates the choice of the multimorbidity measure. The “Core list” (L20) may partially resolve this dilemma, as it demonstrated optimal prediction for many outcomes within the five to ten-year time frame. Moreover, in populations aged 65 years and older, multimorbidity defined as ≥ 3 or ≥ 4 chronic diseases should be preferred to the conventional ≥ 2 diseases, as outcome prediction is typically better for the former. Our results provide a comprehensive assessment that will allow users to select the optimal choices according to the availability of LP in their datasets. These findings will inform the elaboration of a more robust and consensus-based multimorbidity measure relying on health administrative databases.

Impact of the length of lookback periods (1 to 20 years) on multimorbidity prevalence according to the type of multimorbidity definition (≥ 2 chronic conditions [MM2+], ≥ 3 chronic conditions [MM3+], ≥ 4 chronic conditions [MM4+]) and the list of diseases (the “All-inclusive” list (L60) grouped all ICD codes of chronic diseases into 60 chronic conditions; the “Core list” (L20) included 20 chronic diseases associated with a high Disable-adjusted life years (DALY) impact; the “Charlson & Elixhauser” list (L31) combined 31 medical conditions included in both indices). The vertical grey lines delineate the minimal lookback period (10 years) required to reach a more “stabilized” multimorbidity prevalence

Illustration of the length of lookback periods where the predictive performance is maximal. Light-grey areas indicate maximal predictive performance for the ≥ 2 chronic conditions (MM2+) definition, grey-dot-pattern areas for the ≥ 3 chronic conditions (MM3+) definition, and dark-grey areas for the ≥ 4 chronic conditions (MM4+) definition. Shaded areas indicate the length of lookback period where the c-statistic ranged in the standard error interval [± 0.001] of the maximal c-statistic . The vertical grey line delineate the minimal lookback period (10 years) required to reach a more “stabilized” multimorbidity prevalence
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to data confidentiality requirements from the QICDSS.
Abbreviations
International Classification of Diseases
International Classification of Diseases, 9th Revision, Quebec adaptation
International Classification of Diseases, 10th Revision Canadian Coding Standard
list of diseases including a core of 20 diseases
list of diseases including 31 diseases from the Charlson and Elixhauser indices
list of diseases grouping chronic conditions into 60 chronic diseases
lookback period, that is the retrospective period of search for diagnosis codes in administrative data
multimorbidity defined as the presence of at least 2 chronic diseases
multimorbidity defined as the presence of at least 3 chronic diseases
multimorbidity defined as the presence of at least 4 chronic diseases
Régie de l’assurance maladie du Québec
Québec Integrated Chronic Disease Surveillance System
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev sept. 2011;10(4):430–9.
Ryan BL, Allen B, Zwarenstein M, Stewart M, Glazier RH, Fortin M, et al. Multimorbidity and mortality in Ontario, Canada: a population-based retrospective cohort study. J Comorb déc. 2020;10:2235042X20950598.
Ho ISS, Azcoaga-Lorenzo A, Akbari A, Black C, Davies J, Hodgins P, et al. Examining variation in the measurement of multimorbidity in research: a systematic review of 566 studies. Lancet Public Health août. 2021;6(8):e587–97.
Johnston MC, Crilly M, Black C, Prescott GJ, Mercer SW. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health févr. 2019;29(1):182–9.
Simard M, Rahme E, Calfat AC, Sirois C. Multimorbidity measures from health administrative data using ICD system codes: a systematic review. Pharmacoepidemiol Drug Saf Janv. 2022;31(1):1–12.
Juul-Larsen HG, Christensen LD, Andersen O, Bandholm T, Kaae S, Petersen J. Development of the chronic condition measurement guide: a new tool to measure chronic conditions in older people based on ICD-10 and ATC-codes. Eur Geriatr Med. 1 juin. 2019;10(3):431–44.
Lambert L, Blais C, Hamel D, Brown K, Rinfret S, Cartier R, et al. Evaluation of care and surveillance of cardiovascular disease: can we trust medico-administrative hospital data? Can J Cardiol avr. 2012;28(2):162–8.
Nanditha NGA, Dong X, McLinden T, Sereda P, Kopec J, Hogg RS et al. The impact of lookback windows on the prevalence and incidence of chronic diseases among people living with HIV: an exploration in administrative health data in Canada. BMC Med Res Methodol. 6 janv. 2022;22(1):1.
Chen G, Lix L, Tu K, Hemmelgarn BR, Campbell NRC, McAlister FA, et al. Influence of using different databases and « look back » intervals to define comorbidity profiles for patients with newly diagnosed hypertension: implications for Health services Researchers. PLoS ONE. 2016;11(9):e0162074.
Article PubMed PubMed Central Google Scholar
Preen DB, Holman CDJ, Spilsbury K, Semmens JB, Brameld KJ. Length of comorbidity lookback period affected regression model performance of administrative health data. J Clin Epidemiol sept. 2006;59(9):940–6.
Simard M, Sirois C, Candas B. Validation of the combined Comorbidity Index of Charlson and Elixhauser to predict 30-Day mortality across ICD-9 and ICD-10. Med Care Mai. 2018;56(5):441–7.
Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol Juill. 2011;64(7):749–59.
Blais C, Jean S, Sirois C, Rochette L, Plante C, Larocque I, et al. Quebec Integrated Chronic Disease Surveillance System (QICDSS), an innovative approach. Chronic Dis Inj Can. 2014;34(Electronic):1925–6523.
Gamache P, Hamel D, Blaser C. L’indice de défavorisation matérielle et sociale: en bref: guide méthodologique. Institut national de la santé publique du Québec; 2019. p. 16.
Calderon-Larranaga A, Vetrano DL, Onder G, Gimeno-Feliu LA, Coscollar-Santaliestra C, Carfi A, et al. Assessing and measuring chronic multimorbidity in the older Population: a proposal for its operationalization. J Gerontol Ser A-Biol Sci Med Sci Oct. 2017;72(10):1417–23.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. oct 2020;17(10258):1204–22.
GBD 2019 Diseases and Injuries Collaborators. Global Burden of Disease (GBD). [cité 18 janv 2023]. Disponible sur: https://www.healthdata.org/gbd/2019 .
Klabunde CN, Harlan LC, Warren JL. Data sources for measuring comorbidity: a comparison of hospital records and medicare claims for cancer patients. Med Care. 2006;44(10):921–8.
Article PubMed Google Scholar
Parks J, Svendsen D, Singer P, Foti ME. Morbidity and mortality in people with Serious Mental illness. National Association of State Mental Health Program Directors (NASMHPD) Medical Directors Council; 2006. p. 87.
Belzile E, Sanche S, McCusker J, Vadeboncoeur A, Ciampi A, Levesque JF. A measure of emergency department use based on Quebec’s administrative data [technical report]. Montréal: St. Mary’s Research Centre; 2011.
Gaulin M, Simard M, Candas B, Lesage A, Sirois C. Combined impacts of multimorbidity and mental disorders on frequent emergency department visits: a retrospective cohort study in Quebec, Canada. CMAJ. 2019;02(26):E724–32.
Mbuya-Bienge C, Simard M, Gaulin M, Candas B, Sirois C. Does socio-economic status influence the effect of multimorbidity on the frequent use of ambulatory care services in a universal healthcare system? A population-based cohort study. BMC Health Serv Res 6 mars. 2021;21(1):202.
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(Electronic):1531–5487.
Schneeweiss S, Seeger JD, Maclure M, Wang PS, Avorn J, Glynn RJ. Performance of comorbidity scores to control for confounding in epidemiologic studies using claims data. Am J Epidemiol. 2001;154(9):854–64.
Steyerberg EW. Validation in prediction research: the waste by data splitting. J Clin Epidemiol nov. 2018;103:131–3.
Tonelli M, Wiebe N, Fortin M, Guthrie B, Hemmelgarn BR, James MT, et al. Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inf Decis Mak 17 avr. 2015;15:31.
Hvidberg MF, Johnsen SP, Glümer C, Petersen KD, Olesen AV, Ehlers L. Catalog of 199 register-based definitions of chronic conditions. Scand J Public Health Juill. 2016;44(5):462–79.
Kondalsamy-Chennakesavan S, Johnson S, Nicklin J, Land R, Garrett A, Obermair A. Charlson’s index: a validation study to predict surgical adverse events in gynecologic oncology. Gynecologic Oncol 1 mars. 2011;120:S121.
The authors are grateful to all QICDSS team members for their support.
Not applicable. No funding was received.
Institut national de santé publique du Québec, 945, Wolfe, 5e étage Québec, Québec, QC, G1V 5B3, Canada
Marc Simard, Marjolaine Dubé, Véronique Boiteau & Caroline Sirois
Department of social and preventive medicine, Faculty of Medicine, Université Laval, Québec, QC, Canada
Marc Simard & Denis Talbot
Centre de recherche du CHU de Québec, Québec, QC, Canada
Marc Simard, Denis Talbot & Caroline Sirois
VITAM-Centre de recherche en santé durable, Québec, QC, Canada
Marc Simard & Caroline Sirois
The Research Institute of the McGill University Health Centre, Montréal, QC, Canada
Elham Rahme
Faculty of Pharmacy, Université Laval, Québec, QC, Canada
Caroline Sirois
Contributions
MS is a PhD Student and CS and ER are the supervisors. MS, CS, ER and DT designed the study. MS, MD, VB analyzed the data. MS wrote the first draft of the manuscript which was critically revised by CS and ER. The final version of the manuscript was approved by all authors.
Correspondence to Marc Simard .
Ethics declarations
Ethics approval and consent to participate.
The use of QICDSS for surveillance and methodological development in population health surveillance has been approved by the custodians of the databases, the provincial Public Health Research Ethics Board and the Québec Commission protecting privacy and access to information (Commission d’accès à l’information du Québec). Informed consent was not required by law (Bill 5 on health and social services information), since the study was based on anonymized data. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Below is the link to the electronic supplementary material.
12874_2024_2243_MOESM1_ESM.pdf
Supplementary Material 1. Additional file 1 . Schematic illustration of the study design; diseases and ICD codes of each list of diseases
Supplementary Material 2. Additional file 2 . results of supplementary and sensitivity analysis
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Simard, M., Rahme, E., Dubé, M. et al. Multimorbidity prevalence and health outcome prediction: assessing the impact of lookback periods, disease count, and definition criteria in health administrative data at the population-based level. BMC Med Res Methodol 24 , 113 (2024). https://doi.org/10.1186/s12874-024-02243-0
Received : 14 July 2023
Accepted : 08 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s12874-024-02243-0
- Multimorbidity
- Health outcome prediction
- Lookback period
- Administrative Data
BMC Medical Research Methodology
ISSN: 1471-2288
- General enquiries: [email protected]
- Published: 17 January 2023
A scoping review of community health needs and assets assessment: concepts, rationale, tools and uses
- Hamid Ravaghi 1 ,
- Ann-Lise Guisset 2 ,
- Samar Elfeky 3 ,
- Naima Nasir 4 ,
- Sedigheh Khani 5 ,
- Elham Ahmadnezhad 6 &
- Zhaleh Abdi 7
BMC Health Services Research volume 23 , Article number: 44 ( 2023 ) Cite this article
24k Accesses
16 Citations
2 Altmetric
Community health needs and assets assessment is a means of identifying and describing community health needs and resources, serving as a mechanism to gain the necessary information to make informed choices about community health. The current review of the literature was performed in order to shed more light on concepts, rationale, tools and uses of community health needs and assets assessment.
We conducted a scoping review of the literature published in English using PubMed, Embase, Scopus, Web of Science, PDQ evidence, NIH database, Cochrane library, CDC library, Trip, and Global Health Library databases until March 2021.
A total of 169 articles including both empirical papers and theoretical and conceptual work were ultimately retained for analysis. Relevant concepts were examined guided by a conceptual framework. The empirical papers were dominantly conducted in the United States. Qualitative, quantitative and mixed-method approaches were used to collect data on community health needs and assets, with an increasing trend of using mixed-method approaches. Almost half of the included empirical studies used participatory approaches to incorporate community inputs into the process.
Our findings highlight the need for having holistic approaches to assess community’s health needs focusing on physical, mental and social wellbeing, along with considering the broader systems factors and structural challenges to individual and population health. Furthermore, the findings emphasize assessing community health assets as an integral component of the process, beginning foremost with community capabilities and knowledge. There has been a trend toward using mixed-methods approaches to conduct the assessment in recent years that led to the inclusion of the voices of all community members, particularly vulnerable and disadvantaged groups. A notable gap in the existing literature is the lack of long-term or longitudinal–assessment of the community health needs assessment impacts.
The population-based health approach aims to improve the population’s health, promote community resilience and reduce health inequities across the socioeconomic gradient via inter-sectoral partnerships among community groups, government, healthcare systems, and other stakeholders [ 1 ]. One key feature for adopting a population-based health approach is to ensure that it is grounded on a solid understanding of community health needs and assets by triangulating evidence from service providers and community members on services availability, accessibility, utilization and experience [ 2 , 3 ]. The process of identification of unmet health needs in a population is crucial for local authorities seeking to plan appropriate and effective programmes to meet these needs [ 3 , 4 ]. If these needs are ignored, then there is a risk of a top-down approach for providing health services, reflecting what a few people perceive to be the needs of the population rather than what they actually are [ 4 , 5 ].
In this context, community health needs assessment is a means of developing a comprehensive understanding of a community’s health and health needs as well as designing interventions to improve community health [ 6 ]. Though the process of community health needs assessment can be conducted in several ways, the primary purpose is to provide community leaders or healthcare providers with an overview of local policy, systems, and environmental change strategies currently in place and help to identify areas for improvement [ 7 ]. Community health needs assessment can provide them with a more nuanced understanding of the communities they serve, making them aware of pressing issues that require system-level changes and support their efforts for resource mobilization to initiate innovative programmes [ 8 , 9 ]. The process to gather evidence on community health needs can also serve as a springboard to strengthen community engagement [ 10 ].
In general, needs assessments are usually designed to evaluate gaps between current situations and desired outcomes, along with possible solutions to address the gaps. Recently, there has been a trend to move away from framing a community with a deficit perspective (need-based approach) to focus on community assets and resources, called community health needs and assets assessment [ 11 , 12 ]. In contrast to a need-based perspective which focuses on local deficits and resources outside the community, an asset-based perspective focuses on honing and leveraging existing strengths within the community to address community needs [ 12 , 13 , 14 ].
Studies have shown that community health needs assessment is used widely by different users and across different settings [ 15 , 16 ]. However, these studies varied widely in terms of purpose, process and methods of conducting community health needs assessment. Furthermore, the extent to which an asset-based approach is used is unclear, beyond the inclusion in guidance and recommendations. Thus, to support national or local decision-makers to make informed choices about the scope, tools, methods and use of community health needs and assets assessment, this scoping review of the literature aimed at: 1) Providing conceptual clarity on community health needs and assets assessment, 2) Determining for what purpose and with what methods community health needs and assets assessment are used globally, 3) Drawing the lessons learnt from previous experience with community health needs and assets assessment: what works in what context and under what conditions, 4) Documenting evidence of impact of community health needs and assets assessment, 5) Consolidating tools and methods used to collect evidence/data underpinning community health needs and assets assessment processes.
Search strategy
Ten databases, including PubMed, Embase, Scopus, Web of Science, PDQ evidence, NIH database, Cochrane library, CDC library, Trip, and Global Health Library were searched in February and March 2021. The search strategy was developed through discussion with experts in the field of population health, a research librarian, and a narrative review of the literature. Preliminary search terms were developed by the research team to reflect a number of core concepts including needs, population, needs assessment, assets assessment and participation. The search process was performed by a librarian with expertise in the use of literature databases (SK). The search terms were pilot-tested and agreed upon within the research team. The PubMed database search strategy presented in Additional file 1 .
Inclusion and exclusion criteria
Studies that focus on community health needs and assets assessment in terms of concepts, rationale, uses and tools were considered in both high-income countries (HICs) and low-and middle-income counties (LIMCs). We included studies in the review if they met the following criteria: 1) Papers providing conceptual clarity and explaining rationale for community health needs and (assets) assessment (This can be articles describing community health needs assessment or community assets assessment or community health needs and assets assessments at the same time or separately). The terms capabilities/ strengths/ resources can be used in place of assets and were considered.); 2) Papers describing or evaluating experiences implementing community health needs (and assets) assessment in a single site or multiple sites; 3) Methodological papers describing tools/approaches for community health needs (and assets) assessment; 4) Review of the literature on community health needs (and assets) assessment.
Types of papers not include in the review were: 1) Studies without a clear description of the community health needs and (assets) assessment methods, 2) Studies assessed a single dimension (i.e. health outcomes only, or healthcare providers’ capabilities only such as patient surveys, health outcomes dashboard, health facility assessment), 3) Studies related to a single disease or programme, 4) Studies focused only on engaging individual patient in their own care, and 5) Studies were not in English.
Three reviewers participated in the selection of the relevant studies (HR, ZA, NN). The eligibility and relevance of the articles were determined by two reviewers independently using the above predefined criteria. In the event of disagreement, a consensus was found between all the reviewers about the status of the article.
Data extraction
Separate data extraction forms were developed for the extraction of the three main categories of papers: conceptual, empirical and review papers. Totally, 121 empirical papers (including 6 review papers) and 48 conceptual and methodological papers were reviewed. Following topics were extracted for empirical papers: 1) General characteristics including author(s), year of publication, country of implementation, study objective(s) and study method; 2) Community health needs and (assets) assessment framing including rational, definitions of community health needs and (assets) assessment/ needs/ assets/ community, initiator(s) or user(s) of the process; 3) Key steps of the process, collected data, data collection tools; 4) Community engagement and the level of engagement; 5) Use of community health needs and (assets) assessment findings, impact of community health needs and (assets) assessment; 6) Facilitators and barriers. Data extraction forms are presented in Additional file 2 .
Data extraction forms were pilot-tested prior to the implementation. Two authors (ZA, HR) independently performed a pilot data extraction of a random sample of ten original articles. After piloting, the authors assessed the extracted data in relation to the scoping review questions and revised them accordingly. The content of the form was finalized by discussion within the team. Regarding conceptual papers, two authors (NN and ZA) initially extracted data from three randomly selected papers and subsequently refined and amended the form having research team inputs.
Four reviewers extracted included studies independently. The data extracted were cross-checked by one of the authors and mutual consensus resolved discrepancies. Individual data extraction forms of empirical papers were then merged into a single, unifying document used for the interpretation and presentation of the results. Following typical scoping review methods, the methodological quality of the included articles was not assessed systematically, however, only peer-reviewed articles were included in our review process [ 17 ].
Synthesis of results
Following reading and extracting conceptual papers, a preliminary conceptual framework (Fig. 1 ) was developed and discussed and agreed upon by team members. The integrative synthesis of the evidence was employed. Specifically, it involved the narrative description of concepts and definitions, key steps of the community health needs assessment and barriers and facilitators of the implementing community health needs assessment.
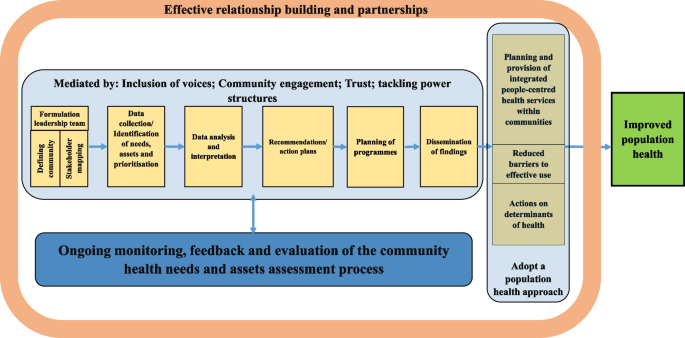
Conceptual framework of the review
The study selection process is summarized in Fig. 2 . Just over 12,000 records were obtained from the ten databases searched. Articles with obviously irrelevant titles were excluded, as were news items, letters, editorials, book reviews, and articles appearing in newsletters or magazines rather than peer review journals. The remaining abstracts were retrieved, read and assessed. A total of 169 articles including both empirical papers and theoretical and conceptual work were ultimately retained for analysis. A list of all studies with a short description, including the year of publication, key focus, study period, and methods, is presented in Additional files 3 and 4 . The first part of the results section focuses on definitions and concepts of community health needs assessment using both conceptual and empirical papers. In the second part of the results section, we describe key steps of the community health needs assessment and tools and methods used to collect data through content analysis of 121 included empirical papers. We also report some important challenges and facilitators faced by included studies while performing community health needs assessment. Role of community participation in the process and the spectrum and types of the participation is discussed in the last part.
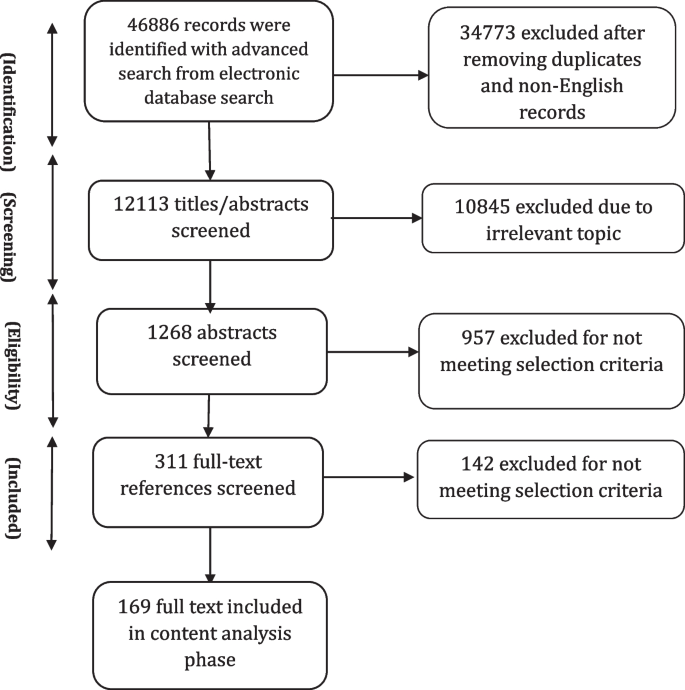
Information flow in scoping review
General characteristics of the included studies
The review showed that community health needs assessment is used widely by different users and across different settings in both HICs and LMICs. Among included empirical studies, 81 (out of 121) were conducted in the United States (US). There were papers from Australia ( n = 4), South Africa ( n = 3), Kenya ( n = 3), Uinted Kingdom (UK) ( n = 2), Canada ( n = 2), China ( n = 2), Dominican Republic ( n = 2), Republic of Ireland ( n = 2), Iran ( n = 2), India (2), Honduras ( n = 1), Netherland ( n = 1), Vietnam ( n = 1), Sudan ( n = 1), New Zealand ( n = 1), Madagascar ( n = 1), Malaysia ( n = 1), Ecuador ( n = 1), Indonesia ( n = 1), Uganda ( n = 1), Taiwan ( n = 1), Kyrgyzstan ( n = 1), Saudi Arabia ( n = 1), Haiti ( n = 1), Honduras ( n = 1) and Korea ( n = 1).
Definition of needs
The review showed “need” was a multi-faceted concept with no universal definition. There was a differentiation between “health need” and “healthcare need” in the reviewed literature. Healthcare needs can benefit from health care (health education, disease prevention, diagnosis, treatment, rehabilitation and terminal care). Healthcare providers usually consider needs in terms of healthcare services that they can supply. However, health needs incorporate the wider social and environmental determinants of health, such as deprivation, housing, diet, education and employment. This broader definition allows looking beyond the confines of the medical model based on health services, to the wider influences on health [ 3 ].
In this review, relatively few empirical studies focus narrowly on healthcare needs, without attention to other determinants of health that can affect health [ 18 , 19 , 20 , 21 , 22 , 23 ]. Most of the included empirical studies looked beyond “physical health needs” to consider wider “social determinants of health” or non-medical factors that can affect a person’s overall health and health outcomes as the conditions—shaped by political, social, and economic forces—in which people are born, grow, live, work, and age [ 24 ]. Notably, the need was recognised as a “dynamic concept” whose definition will vary with time according to context and resources available to address these needs [ 16 ].
Definition of community
In general, “community” has been defined as “people with a basis of common interests and network of personal interactions grouped either based on locality or on a specific shared concerns or both” [ 25 ]. Shared common interests are particularly important as they can be assessed and, hopefully, met at a community level [ 26 ]. Importantly, community is a dynamic concept as individuals can belong to several communities at various times. In our review, community was defined by included studies, particularly those initiated by local authorities or healthcare providers (e.g., hospitals), based on geographical indicators such as county designations or based on the location of the hospital’s/facility’s/authority’s existing or potential service users. Some included empirical studies considered community based on shared interests or characteristics such as race/ethnicity, sexual orientation, or occupation. Medically underserved populations including rural areas [ 27 , 28 , 29 , 30 ], impoverished urban sectors [ 31 ], the homeless [ 32 , 33 , 34 , 35 ], persons in poverty or of low socioeconomic status, vulnerable children and families [ 18 , 28 , 36 , 37 , 38 ], the elderly [ 8 , 39 , 40 , 41 , 42 ], women and girls [ 43 , 44 , 45 , 46 , 47 ], LGBT (Lesbian, gay, bisexual, and transgender) individuals [ 48 , 49 , 50 , 51 ], displaced populations, immigrants and racial, ethnic and religious minority groups [ 12 , 19 , 36 , 42 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 ] and persons with severe and chronic health problems [ 79 ] were considered as a “community” by a number of included studies.
While defining community, a number of its characteristics were determined by included studies including: history, existing groups, physical aspects (i.e. geographic location, community size, its topography and etc.), infrastructure (i.e. health and social care facilities, public transportation, roads, bridges, electricity, mobile telephone services and etc.), demographics (i.e. age, gender, race and ethnicity, marital status, education, number of people in household, first language and etc.), economic conditions, deprivation and/or inequalities, government/politics, community leaders (formal and informal), community culture (formal and informal), existing institutions, crime and community safety, lifestyle and leisure, general health problems and epidemiology.
In our review, community health needs and assets assessment were performed by different organizations as the first step in community health promotion planning, including local health authorities (district/local), community entities [i.e. non-governmental organizations (NGOs), civil society organizations (CSOs), faith-based organizations (FBOs), community-based organizations (CBOs)] and hospitals (public/private). Included studies mostly conducted health needs assessment at the local level (e.g. cities, counties, or other municipalities). The broader understanding of health and its determinants suggests that many public and private entities have a stake in or can affect the community’s health. To engage stakeholders in the process, a number of included empirical studies ( n = 56, 49%) sought representatives from the community that were best positioned to speak about community health based on their specific knowledge or line of work. These stakeholders were individuals from community and entities who may explicitly be concerned with health or not, which varied by the community context and culture. To have a comprehensive overview of a community needs, it was asserted that defining communities needs to be dynamic and socially constructed to take into account all voices and members, especially those not ordinarily included [ 80 ]. Community should be defined in a manner that does not exclude medically underserved, low-income, or minority populations. Integrating community voices is especially important in designing plans and programmes aimed at reducing health disparities in the community [ 58 , 81 , 82 ].
Definition of assets
Overall, there were limited definitions for “community assets” in the reviewed literature. Assets were described as resources, places, businesses, organizations, and people that can be mobilized to improve the community [ 11 , 83 ]. This includes members of the community themselves and their capabilities. Assets can therefore be described as the collective resources which individuals and communities have at their disposal, which protect against adverse health outcomes and promote health status [ 83 , 84 ].
Of 115 included empirical studies, 30 studies addressed community assets while performing community health needs assessment. A wide range of assets, from tangible resources to intangible ones, were considered that can be classified into seven broad categories as follows:
Community demographic characteristics: Literacy rates [ 13 ], youth population [ 58 , 68 ], and elderly population [ 68 ];
Natural capitals: Geographical location and natural resources [ 21 , 81 , 85 ];
Economic and financial capitals: Community business [ 12 , 81 ] community members’ income [ 21 ], and housing land ownership [ 13 ];
Community infrastructure: Level of technology/mobile phone coverage [ 13 , 21 ], transportation [ 86 ], parks and sidewalks [ 12 ], sport and recreational facilities [ 31 , 87 , 88 ], public libraries and community centres [ 88 ];
Community social and educational facilities: Non-profit and non-governmental organizations [ 59 , 87 ], media [ 89 ], educational institutions [ 12 , 31 , 81 , 90 ], faith communities [ 58 , 81 , 90 ], and community associations [ 31 ];
Community health and social facilities: Health and social facilities and providers [ 72 , 81 , 85 , 86 , 89 ], traditional medicine providers [ 72 ], and ongoing health programmes [ 13 , 87 ];
Community’s social and cultural values and resources: Tribal and community culture [ 58 , 68 , 74 , 91 ], cultural diversity [ 81 ], spirituality and religion [ 58 , 74 ], strong family bonds and values [ 59 , 74 ], strong community connections, teamwork and willingness to volunteer [ 21 , 81 , 86 , 91 ], mutual support, social support and networks [ 45 , 58 , 81 , 85 ], unity, community cohesion and collectivity [ 21 , 59 , 74 ], community capacity [ 58 ], community-led activities [ 86 , 91 ], and community values and traditions [ 68 , 74 , 86 ], resiliency [ 58 ], unifying power of communities [ 13 ], community administration units e.g. women’s committees [ 13 ], an existing group of dedicated healthcare providers [ 39 ], a group of concerned citizens [ 39 ], community safety [ 12 ], the knowledge base of the community members themselves [ 39 ] and members’ desire to be healthy [ 58 ].
Various qualitative methods such as individual interviews (one-on-one structured conversations) or focus groups (guided, structured, small group discussions) with community members, or key informants’ interviews (formal and informal conversations with leaders and stakeholder groups) or a combination of these methods were reported as the main methods to collect information on community’s assets among reviewed studies. Of these, focus group was the widely used method in community assets assessment [ 8 , 21 , 31 , 45 , 58 , 59 , 67 , 81 , 82 , 85 , 87 , 90 , 92 , 93 ].
Definition of community health needs (and assets) assessment
The terms “Community Needs Assessment (CNA)”, “Community Health Needs Assessment (CHNA)”, and “Community Health Needs and Assets Assessment (CHNAA)” were used interchangeably in the literature referring to the process of identifying health needs (and assets) of a given community. Since this review focuses on both community needs and assets, we will use the CHNAA term for the description of the process in this paper.
None of the papers reviewed provided a specific definition for CHNAA. In general, reviewed papers defined CHNAA as: A collaborative, community-engaged, systematic, ongoing, continuous, proactive, comprehensive, cyclical, regular, modifying method or process [ 28 , 33 , 69 , 92 , 94 , 95 , 96 , 97 , 98 ]; For the identification, collection, assembly, analysis, distribution, and dissemination of information on key health needs, social needs, concerns, problems, gaps, issues, factors, capabilities, strengths, assets, resources; About communities (or individuals) [ 21 , 23 , 28 , 31 , 33 , 37 , 41 , 45 , 54 , 79 , 89 , 94 , 95 , 96 , 97 , 99 , 100 , 101 , 102 ]; To achieve agreed priorities, create a shared vision, plan actions, garner resources, engage stakeholders, work collaboratively, establish relationships, implement culturally appropriate, multi-sectoral/multilevel intervention strategies, empower residents and enhance community capacity and participation in decision-making process [ 12 , 13 , 20 , 27 , 28 , 37 , 45 , 70 , 79 , 89 , 91 , 92 , 94 , 95 , 97 , 98 , 99 , 101 , 102 , 103 , 104 ]; Towards improving health and wellbeing, building and transforming health of the communities, increasing community benefits, reducing inequalities; Through which primary/secondary healthcare can respond to local and national priorities [ 20 , 23 , 28 , 40 , 51 , 59 , 69 , 97 , 103 , 105 , 106 ].
The included studies listed a number of reasons as the rationale for conducting CHNAA. Legislative requirements were most cited as the main rational for conducting CHNAA, particularly among studies conducted in the UK and US. Since the late 1980s, the concept of health needs assessment has gained increasing prominence within the National Health Service (NHS) in the UK. This has been prompted by a series of policy initiatives requiring health facilities to assess needs of their populations and to use these assessments to set priorities to improve the health of their local population [ 107 , 108 ]. In the US, several national, federal, state, and local funding sources require entities to conduct CHNAA to demonstrate a significant need for their services and programmes to be funded. The most important one is Patient Protection and Affordable Care Act (ACA-2010), requiring non-profit hospitals as tax-exempt entities to perform CHNAAs to maintain non-profit status regularly [ 92 ]. Other reasons were mentioned by included studies as the rationales for conducting CHNAA were: lack of information of health needs of a specific community, to facilitate health research and related interventions in a community, to inform the design of contextually relevant programmes and policies, to develop community health improvement plans or health promotion interventions, to develop or update strategic plans, and to receive resources and funds.
Key steps to conduct CHNAA
The number and nature of CHNAA process steps varied among reviewed studies. However, broadly CHNAAs involved six main steps as follow:
Formulation of a leadership team
Forming a leadership team, which was called by different names such as the steering committee/ the research advisory committee (RAC)/ the collaborative task force/ or the community advisory board (CAB), was known as the preliminary step of a CHNAA process. The steering committee was usually composed of local representatives from local agencies and organizations (e.g. non-profit organizations, community service agencies, media outlets, county and municipal governments, colleges and universities, faith-based organizations, and healthcare providers), community members, community stakeholders and leaders, academic partners, health and social officials, and representatives from the investigator body to help guide the development of the CHNAA project.
Leadership team responsibilities were reported as providing inputs on the research purpose, selecting and verifying study methodology and design, providing inputs and feedback on initial survey/topic content and selecting final survey/ topic guide questions, reviewing survey/topic guide length, and ensuring culturally relevant and resonant wording, comprehension and face validity, and monitoring the progress of the data collection. Feedback and recommendations from the steering committee were incorporated throughout the CHNAA process as well. Steering committees usually met on a regular basis.
Identification of needs, assets and prioritisation
To collect information on community health, needs and assets, both primary and secondary data were utilized by included studies. Secondary data included information on community socio-demographic and indicators on health status, access, utilization and satisfaction with health and social services at different levels (e.g. community, sub-national and national) to develop a picture of the overall community health. Primary data were collected through quantitative and qualitative methods and mixed-methods approaches.
Quantitative studies
Some empirical studies used individual/household surveys as the only source to identify community needs and concerns ( n = 28, 24.%). Surveys were a popular method of gathering opinions, preferences and perceptions of needs. Needs assessment surveys typically have written, closed-ended questions filled through the interview (face to face/telephone) or self-completion (paper or online) by community members. Generally, two main kinds of surveys were used by included studies: a) community health assessment survey, and b) community concerns survey. A number of included studies used health assessment surveys as the key data sources of the CHNAA process ( n = 22, 19%) or along with other types of data, mainly qualitative data ( n = 21, 18.%). Health assessment surveys typically collected information on demographics, socio-economic variables, respondents’ health status, choice of healthcare providers, and healthcare access issues among community members. Survey questionnaires were mostly developed with inputs from the literature review (similar health assessment surveys conducted at the local or national level), community members and project team discussions. Additional file 5 shows the most important data and indicators collected by included studies through conducting community health assessment surveys.
Another form of surveys, used alone or in combination with qualitative methods ( n = 15, 13.5%), was the community concerns survey in which people (community members and/or key informants) are asked to help identify what they see as the most important issues facing their community leading to an inventory of their health priorities [ 12 , 20 , 23 , 27 , 29 , 55 , 69 , 74 , 101 , 103 , 109 , 110 , 111 , 112 , 113 ]. A straightforward way to estimate the needs of a community was to simply ask residents their opinion on what particular services are most needed in the community. The focus of this methodology was to create an agenda based on the perceived needs and concerns of community residents. The concerns surveys were based on either focus group discussion with community members and experts or literature review by the researchers or both. Generally, while filling community concerns survey, individuals were asked to rate the importance of each issue in their community on a scale (e.g. 0 = not important, 5 = extremely important) [ 23 , 27 , 29 , 55 , 74 , 110 ]. Participants could also add and rate concerns or service needs that were not listed. Finally, each health problem identified by the community was weighted based on the frequency it was selected on the survey.
General coverage of the surveys was the population aged 18 or over currently residing in the community for a minimum period of time (at least a few months) and able to provide consent for participation. Most surveys were written, closed-ended questions filled through face to face or telephone interviews or self-completion by community members. In addition to the paper-form survey, some studies used email and social media platforms to allow residents to anonymously complete online surveys [ 29 , 51 , 57 , 96 , 103 , 110 , 114 ]. A few studies reported that residents received monetary or nonmonetary incentives for their participation upon survey completion [ 19 , 71 , 74 , 77 , 110 ]. Sampling techniques commonly used are those that promote participation in CHNAAs such as convenience sampling [ 20 , 35 , 40 , 51 , 52 , 57 , 64 , 65 , 71 , 74 , 75 , 77 , 86 , 96 , 101 , 103 , 104 , 110 , 114 , 115 ]. Only a few studies used random sampling or demonstrated the representativeness of their samples. Their response rates varied between 8 to 95.5%. Most surveys recruited local surveyors and provided them with research training to ensure consistent survey administration to attract community participation. Some studies that assessed health needs among immigrant communities or minority groups recruited bilingual surveyors or/and provided participants with two versions of the instruments, one in the native language to maximize community engagement [ 12 , 27 , 52 , 65 , 71 , 86 , 103 ]. Surveys that took a participatory approach to the design, content, terminology, and language level, were reported more understandable and culturally relevant to the community members [ 52 , 65 , 75 ].
Health needs assessment surveys (both concerns surveys and health assessment surveys) reported limitations to data collection based on the assessment timing, data availability, and sample response. As said earlier, using a convenience sampling and non-representative samples, small sample size and inter-rater reliability between surveyors were among some important methodological limitations reported by these studies, which limited the generalisability of the study findings to the entire community population [ 35 , 57 , 65 , 71 , 74 , 75 , 77 , 96 , 106 , 116 ]. Convenience sampling method and using community events as sampling sites led to sampling bias in some studies (e.g., an over-representation of some specific groups of the population such as women and low –income or high-income groups) [ 57 , 63 , 65 , 66 , 71 , 74 , 75 , 78 , 103 , 114 , 115 ].
Qualitative studies
Among included studies, about 34% ( n = 39) used qualitative methods as the main source of data collection on community needs and assets. Some of these studies justified the use of qualitative approach by explaining how the overreliance on quantitative, population-level data resulted in CHNAAs failing to identify health needs and interests of all community members, particularly those of vulnerable population and underrepresented marginalized segments of the community. In addition, these studies concluded that integrating qualitative methods into the CHNAA process has the potential to involve community members in a more participatory fashion, perhaps improving future collaborations between communities and service providers. Such collaborations can help to design focused initiatives, making them more meaningful and culturally appropriate [ 12 , 59 , 91 , 102 ].
Key informant interviews, individual interviews with community members, focus groups with community members and community forums were among the qualitative data collection techniques used individually or in combination with each other by these studies to collect data on community needs and assets. They asserted that qualitative techniques specifically targeted to underrepresented segments of the population proved to be effective mechanisms to explore the participants’ perceptions on issues surrounding community health needs and assets. The most used technique to elicit community members’ opinions were focus group discussions and key informant interviews.
Small sample size and single-site setting were mentioned as the most cited limitations of the qualitative CHNAAs that limit these studies generalisability. Because the studied communities were unique communities with unique assets, constraints, and health needs, the CHNAA findings cannot be generalised to other communities [ 32 , 39 , 62 , 70 , 72 , 73 , 91 , 117 , 118 ]. Another limitation mentioned by some studies was that the demographic composition of the focus group participants, specifically with regards to race, gender, socio-economic status and age group, did not fully reflect the population of studied community as a whole [ 13 , 61 , 62 , 72 , 97 , 119 ]. Some studies reported that they could not include all influencing key informants in the community to facilitate broader understandings of health needs [ 13 , 120 ].
Mixed- methods studies
A variety of data collection methods were used in a number of included studies to ensure that a comprehensive picture of community health needs and resources was obtained ( n = 48, 42%). Some of these studies were two-phase explanatory mixed-methods studies, with the quantitative phase preceding the qualitative phase ( n = 14, 12%). They conducted targeted focus groups or community listening sessions or interview with community members/key informants following needs assessment survey to supplement the findings from the survey and provide further information about health status, needs of daily living, barrier to health and access to community resources [ 8 , 21 , 41 , 53 , 55 , 66 , 67 , 93 , 94 , 95 , 99 , 113 , 114 , 121 ]. In addition to these studies, some studies used triangulation mixed-method design to obtain complementary qualitative and quantitative data on community health needs and issues ( n = 13, 11%). These studies confirmed that using multiple data sources ensured researchers obtain a complete picture of the community health needs. Applying qualitative methods in the form of focus groups and semi-structured interviews enabled exploration of problems and needs within their social context and provided a wider perspective on issues raised. However, to conduct such studies CHNAA teams had to have members who have qualitative and quantitative expertise. There were some limitations specific to the mixed-method studies, including lack of rigor in integrating qualitative and quantitative findings, relying heavily on quantitative data for health need determination, and absence of the voices of the communities most in need [ 69 , 91 ].
Data analysis and interpretation
Qualitative data from focus group discussions and key informant interviews were mainly audio-recorded and transcribed verbatim by the research team and all identifying information was removed. Different analytical approaches, mostly content analysis and thematic analysis, were used to identify main themes related to assets, needs and gaps in the service system and priority populations.
Quantitative data from surveys were analysed using statistical software. Descriptive statistics were used to describe the sample in terms of socioeconomic background and present the prevalence of chronic diseases, risk factors, and health behaviours. Statistical analytical tests were also used to compare results between different groups of community members. Results also were compared by those at the state/ national level or from a similar community. Those diseases or risk factors that had a high prevalence among community members are regarded as priorities that to be addressed further.
Formulation of recommendations across various levels (individual, institution, community, policy levels)
Following analysis of the quantitative and qualitative data, the studies included in the review provided a thorough list of health needs and assets of the community. Included studies mainly used CHNAA outputs: 1) as a resource to provide baseline data of community’s health; 2) as a resource to prioritize and plan services; 3) as a resource for writing grant applications; 4) as a resource to guide a comprehensive health promotion strategy.
Not all included CHNAAs proposed interventions to address identified needs and issues. Some of the included studies ( n = 45, 39%) just provided a snapshot of the most important issues faced by the studied community. They demonstrated several areas where CHNAAs provide more information to researchers, community organizations, and policy-makers. On the other hand, not all identified issues and needs were addressed by those studies performed CHNAA in order to implement interventions or strategies. In practice, specific populations or a number of specific health conditions or health risks, or overarching issues such as health inequality and disparities were prioritized by these studies.
In most cases, decisions on implementation were carried out by the CHNAA steering committees or the research teams. Only a number of studies used a clear and explicit set of criteria for deciding the importance of each issue [ 22 , 27 , 43 , 67 , 94 , 118 , 122 ]. A wide range of criteria were used by included studies such as: impact, urgency, community concern, achievability within the set time [ 94 ], seriousness, urgency, solvability, and financial burden of the problems [ 27 ], perception of survey participants on importance of the identified issues and feasibility of intervention, prevalence, fatality, social and cultural stigma [ 22 ], possible interventions, organizational capacity, and community assets and resources [ 13 ], importance and possibility of the effecting change [ 43 ], prevalence, impact on the duration of sickness, impact on mortality, and the availability of treatment [ 122 ], impact of the problem on the overall wellness, quality of life, and resources of their community [ 118 ], factors of health issue, size, seriousness, and effectiveness of available interventions [ 101 ], importance and feasibility [ 67 ].
Different techniques for ranking priorities were applied by included studies such as: 1) Multi-voting technique (decide on priorities by agreeing or disagreeing in group discussions and continuing process/rounds until a final list is developed), 2) Strategy lists (determine if the health needs are of “high or low importance” by placing emphasis on problems whose solutions have maximum impact, with the possibility of limited resource), 3) Nominal group technique (rate health problems from 1 to 10 through group discussion), and 4) Prioritization matrix (weigh and rank multiple criteria for prioritization with numeric values to determine health needs with high importance).
Overall, health priority types were categorized into four main categories by included studies:
Medical conditions (e.g. obesity, diabetes, heart diseases, asthma, mental health disorders, substance abuse, vision/ dental problems, HIV/AIDS and sexually transmitted diseases, injuries and health consultations).
Health behaviours (e.g. physical activity, eating habits/ nutrition, tobacco consumption, teen pregnancy and violence/gangs).
Community conditions (e.g. poverty and unemployment, environmental and infrastructural conditions, such as air quality/pollution, transportation, access to clean water and sanitation, community collaboration, and access to healthy food, exercise facilities and occupational concerns).
Health systems priorities (e.g. access to care, including primary care and higher levels of care, specialty care, mental/ behavioural health care and dental care, quality and acceptability of health services, lack of cultural competence in health systems, flexible hours and waiting time).
However, guided by a community-based participatory research (CBPR) approach, a number of studies involved community members and stakeholders in priority identification or ranking [ 12 , 21 , 22 , 23 , 27 , 29 , 31 , 36 , 41 , 43 , 49 , 53 , 55 , 56 , 58 , 59 , 60 , 62 , 63 , 68 , 70 , 74 , 86 , 87 , 88 , 90 , 92 , 99 , 100 , 103 , 104 , 110 , 114 , 117 , 118 , 119 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 ], in potential strategy selection [ 13 , 19 , 67 , 82 , 89 , 130 ], and in carrying out strategies [ 8 , 37 , 69 , 81 , 93 , 105 , 113 ]. They asserted that by involving the perspectives of the relevant stakeholders, a comprehensive overview of the issues and possible effective solutions was created.
Planning of programmes and interventions, implementation and evaluation
The results of CHNAA were used in various ways by included studies. In some studies, particularly researcher-led studies with limited support or involvement of the local authorities, CHNAA just led to the identification of new, locally relevant issues and priorities without any further actions ( n = 45, 39%). The results of these CHNAAs provided more information to researchers, community organizations, and local policy-makers. Their results also may guide further research agenda in the community [ 18 , 21 , 23 , 29 , 35 , 39 , 40 , 42 , 44 , 48 , 49 , 50 , 52 , 54 , 55 , 62 , 64 , 65 , 66 , 69 , 70 , 71 , 72 , 73 , 76 , 77 , 78 , 85 , 96 , 106 , 122 , 123 , 131 , 132 , 133 , 134 , 135 ]. Some of these studies tried to present their results to the local authorities through various channels in the hope that it would modify existing programmes or implement new ones to meet the needs of the community residents. In addition to identification of relevant issues and priorities, included studies listed at least one outcome associated with the reported CHNAA activity as follows:
Development or modification of health and social policy and programmes: The knowledge provided by CHNAAs helped develop better tailored, and thereby potentially more effective interventions by a number of studies. Further, the information gathered from the CHNAA process was used as the baseline against which to measure future targets for assessment efforts and progress in areas were targeted ( n = 36).
Formation of new partnership: In some cases, a new partnership among entities involved in CHNAA was formed to address health issues. One of the partnerships reported successful was the community–academic partnership in which communities used the research capacity of academic institutions to conduct the CHNAAs ( n = 20). Another type of the partnership reported by some studies was the collaboration among healthcare organizations serving the same geographic area to conduct CHNAA jointly. Conducting a joint CHNAA may avoid duplication of planning efforts and obviate the creation of multiple community health needs assessments for the same population ( n = 5).
Development of new recommendations: Several suggestions were proposed to be considered while designing health improvement interventions in the future by some of the included studies ( n = 18).
Setting or altering strategic direction: Strategic agency direction was established or altered in some cases, which might indicate that the CHNAA was used to redirect resources better to meet the needs of the community ( n = 4).
Raising awareness about health issues: One of the most important insights brought by CHNAA findings was the recognition of the health priorities and contributing factors by the community members, leaders and researchers, leading to an increased awareness of community issues among them ( n = 8).
Engaging and motivating policy-makers and stakeholders: A few studies reported that CHNAAs provided health organizations with the opportunity to identify and interact with key policy-makers, community leaders, and key stakeholders about health priorities and concerns, which might foster a sense of collective ownership and trust in the results and increase the likelihood that the CHNAA will be used ( n = 5).
Having an impact on obtaining resources and resource allocation: The CHNAAs provided the community partners with locally relevant information regarding the current status of health and perceived community needs to inform resource allocation and applications for new grants for the initiation of new programmes ( n = 14)
Contribution to the development of CHNAA process: Some studies reported that the specific methods used in their CHNAA processes could contribute to more relevant and effective community health need assessment process ( n = 10).
Dissemination of findings
Disseminating of the findings and knowledge gained to all partners involved was a foremost step of CHNAAs. The most cited product of the CHNAA process in the included studies was the community needs assessment report. This report includes information about the health of the community as well as the community’s capacity to improve the lives of residents. The report provides the basis for discussion and future actions. In addition to the final report, other channels to disseminate CHNAAs findings were reported as: publishing CHNAA main results in local newspapers, communicating research results with community members and stakeholders in public forums or meetings, presentation results to the steering committee and various stakeholders, posting the report on the local authorities websites, individual meetings with community leaders and stakeholders, posters, and presentation of findings in academic conferences.
Community participation
Among included studies, around 50 studies (44%) reported using participatory approaches and techniques to encourage community members' participation in CHNAA process. Unlike traditional approaches to health needs assessment, participatory approaches aimed to incorporate community inputs at all stages of the research process to enhance capacity building and overcome barriers to research raised by matters of trust, communication, cultural differences, power and representation. A variety of participatory approaches (e.g. community based participatory research (CBPR), participatory rural appraisal, participatory action research (PAR), rapid participatory appraisal (RPA), tribal participatory research, community-based collaborative action research (CBCAR), precede-proceed model, concept mapping and photovoice) were used by these studies to ensure that communities participate in CHNAA, from defining the community to identifying needs and assets and developing new interventions.
Pennel and colleagues classified the depth of the community participation in CHNAA activities into four main categories [ 136 ]. In this classification, depth of the community participation was assessed by the types of activities in which participants were involved throughout the assessment and planning process as follows:
No participation: No attempt to engage community stakeholders or members;
Consultation-only: Engagement of health-related stakeholders, broader community stakeholders, and/or community members to identify health needs through surveys, interviews, and/or focus groups; verified or validated health needs/priorities with local experts;
Moderate participation: Involvement of community stakeholders/ or community members in priority identification; involvement of community stakeholders in strategy selection;
Extensive participation: Involvement of community stakeholders/or community members to develop and carry out strategies.
The above classification was used to assess the depth of the community participation by included studies. Based on the content analysis, community participation in CHNAA process varied considerably across the included empirical studies, from minimal to in-depth participation (Table 1 ). Around 65% of the included studies were involved in consultation-only to identify health needs through one-way communication using tools such as surveys, interviews, and focus group to identify community needs and resources. Around 22% of the included studies solicited moderate participation from the community by involving community in verifying needs and final priority selection and only about 10% of the included studies reported a broad and deep community participation including community involvement in designing and implementing strategies to improve community health.
Three categories of challenges were cited by the reviewed studies while performing CHNAA projects.
Methodological challenges: These are mainly associated with quantitative and qualitative data collection methods, which were discussed earlier. Other methodological challenges cited were: difficulties in aggregating and making sense of data collected from various sources (triangulation), non-generalisability of site-specific data and limitations of the use of existing epidemiological data alone, which does not provide a comprehensive view of health needs, yet is often the most available source of information. Traditional approaches to data collection were challenging where language and literacy barriers existed [ 12 , 52 , 65 , 71 ]. Another major challenge reported by studies used community-based participatory research approaches was the challenge of involving the community in decisions related to research design and data collection methods while maintaining an appropriate level of methodological validity and reliability [ 56 , 81 , 121 ]. In addition, participation was not without challenges. Including the perspectives of stakeholders and residents can lead to differing accounts of what services are seen as essential, and each party may push their own agenda based on their personal or professional interests. Further, linguistic and cultural barriers may be a major factor among minority groups hindering participation in such endeavors [ 81 , 137 ].
Logistical challenges: The major logistical challenges reported were the need for a considerable amount of time (often inadequate), and resources required to conduct a comprehensive assessment [ 80 , 138 ]. Good quality local data on the needs and utilization of health services are usually difficult to obtain [ 9 ]. Financial costs are considerable and the depth of information obtained will ultimately depend upon the methods employed [ 139 , 140 ]. In addition, health professionals, managers and others involved in health services planning and delivery may not have the requisite skills to conduct CHNAAs. This goes beyond technical skills and places an emphasis on soft skills and flexibility including good listening skills, the ability to establish trusting relationships, empathy, working with diverse groups and reflexivity [ 140 , 141 ]. Moreover, limited health information infrastructure and systems in developing countries settings may have hindered the availability of good quality information to conduct CHNAAs [ 13 , 28 , 30 , 142 ].
Ethical challenges: Concerns were raised about the ethical issues associated with community consultation about felt needs followed by priority setting process that leaves many needs unaddressed and the bulk of expectations dashed. Labelling, stigma and stereo- typing are other problems raised by needs assessment [ 143 ]. Needs assessment results may not be utilised, leaving unmet expectations and may require extensive financial and political support to lead to changes in health service planning and delivery [ 9 ]. Comprehensive health needs assessment is likely to produce different, potentially conflicting needs, exposing hidden conflicts and tensions in communities without any mechanisms to address these issues [ 5 ]. Further, local participation may only allow those who are able to voice their needs to do so, leaving behind the silent or hidden voices [ 81 ]. Involvement of the community in the needs assessment process also impacts upon possible outcomes of the project especially since it is likely that expectations of changes to programmes and service delivery may have arisen from local participation [ 144 ].
Facilitators and enablers
CHNAA projects need to be organized in such a way that they have clear objectives, and are adequately resourced by experienced staff. In addition, factors such as clear objectives, decisive leadership, teamwork, communication, sound study design, adequate resourcing, skilled staff, sufficient time and ownership by stakeholders are among those factors that contribute to the successful implementation of CHNAAs [ 15 , 145 ]. Most studies cited community participation as a major facilitator of the CHNAA process and outcomes. Participation was shown to foster bidirectional learning and communications, where both health authorities and the community learnt about needs and priorities. Different benefits for community engagement were mentioned by reviewed literature including, improved participants’ recruitment, enhanced capacity among stakeholders, productive conflict resolution, increased quality of outputs and outcomes, increased sustainability of project goals beyond funding and timelines and development of linguistically and culturally appropriate measures. In addition, incorporating community voices has the potential to inform the development of sound measures to tackle health disparities in the basis of race, social class and ethnicity [ 12 , 27 , 30 , 91 , 103 , 110 , 126 , 146 ].
The main objective of our scoping review was to provide an overview of why and how community health needs and assets assessments (CHNAAs) have been used globally. Substantial variation was found among the studies reviewed concerning definitions, process, participants, methods, goals, and products, yet there were many common characteristics.
Some CHNAAs focused narrowly on health care in assessing needs, with scant attention to other community issues that can affect health. However, most of the included studies looked beyond health needs and considered social and environmental conditions influencing community health. We argue all CHNAAs should approach community health needs assessment holistically, focusing on both individual physical and mental wellbeing as well as casting a social determinants of health lens on the population health.
The review showed that community health needs assessment is used widely by different users and across different settings in both HICs and LMICs. However, in countries such as the US it has become institutionalized and has accordingly been developed, as service providers, particularly hospitals, are mandated to perform CHNAA to compliance with legislative mandates. However, though federal and state laws impose requirements on hospitals to conduct CHNAAs, the methods for needs assessments are generally left to the discretion of each hospital [ 147 ]. As a result, assessment methods vary widely. US-based CHNAAs either develop their own CHNAA processes or utilize a process developed at the state or national level to guide their efforts. A number of toolkits have been provided by different organizations across US to help healthcare providers to conduct CHNAA projects [ 6 , 148 , 149 ]. This highlights the need for consensus guidance across many countries and settings while maintaining the responsiveness to contextual needs, assets and priorities.
Both qualitative and quantitative approaches were employed to collect data on community health needs and assets. Overall, there has been a growing use of mixed-methods approaches to conduct CHNAA in recent years, owing to the recognition in the literature that using qualitative and quantitative approaches simultaneously can provide complementary insights determining community health needs and assets [ 69 , 91 , 104 ]. Although quantitative approaches yield concrete evidence of community needs and assets, qualitative approaches provide a context for how these issues can be addressed using available resources [ 91 , 102 ]. Using qualitative methods in conjunction with more traditional quantitative approaches is especially appropriate for studying complex public health issues and promotes the alignment of implementation plans with the local needs of community members [ 59 , 69 , 91 ]. The growing use of mixed-methods approaches has practical implications for research training and capacity building within entities performing CHNAAs. Organizations who wish to conduct CHNAAs will need to ensure that the competencies and expertise required for mixed-methods studies are available.
Although only a small number of studies provided definitions of assets, there is a growing interest in the literature in asset-based assessment, which examines and mobilizes community assets, instead of focusing on only the needs of communities [ 11 , 84 ]. Unlike need-based or deficit approaches, asset-based approaches document resources and focus on strengths to enhance and preserve rather than deficits to be remedied. Related to principles of empowerment, it postulates that solutions to community problems already exist within a community’s assets. By recognizing existing capacity, communities can become empowered to take ownership of their health and improve as a population [ 11 , 31 , 125 ]. An asset-based approach was recognized as essential for enhancing trust and community coalitions [ 83 ]. Further, it is more participatory in nature through involving community stakeholders throughout the needs assessment process [ 82 , 83 ]. In particular, it highlights community resilience, resources, and opportunities for positive growth rather than focusing solely on health problems or other concerns [ 14 , 84 , 88 ]. In developing countries, assets identified from within the community are crucial for later use in the implementation of health programmes. The shift from a traditional needs-based perspective to an asset-based perspective to health needs assessment can help to address resource constraints in these countries [ 13 , 30 , 150 ].
There was a growing interest in the use of participatory approaches and in their value in identifying and addressing community health needs over recent years among included studies. About half of the reviewed studies applied CBPR or other community-engaged approaches to perform CHNAA. There are several opportunities to fully engage patients, families, and communities in healthcare delivery redesign to ensure that they are provided in a way that address the community members’ needs and preferences. The CHNAA process is one mechanism for this engagement—and a good precursor to deeper engagement and collaboration [ 91 , 97 , 123 ]. Integrating community voices into CHNAA process may be crucially important for confronting health disparities at the community level, which stemming from socio-historical processes, including racial and ethnic discrimination and economic inequality [ 33 , 74 , 86 , 91 ]. To eliminate health disparities, it is critical first to understand social, cultural, and economic determinants of health. CHNAAs, particularly when they include the voices of community residents, can provide an opportunity to understand local processes contributing to health disparities. This knowledge can then be used to inform health and equity initiatives [ 91 , 110 , 126 ]. The development process and implementation of a CHNAA project is an important example of evidence-based public health practice. It is a way to address health and health care disparities experienced by medically underserved populations [ 86 , 92 , 126 ]. Those studies used a participatory approach reported that by having community participation, concerns and issues of the most marginalized and vulnerable populations were voiced. The inclusion of these voices allowed for a broader and deeper understanding of the concerns of those who are typically marginalized and that may be missed in traditional health needs assessment methodologies [ 33 , 56 , 58 , 74 , 86 , 110 , 137 , 146 ]. Hence, defining communities while performing CHNAA needs to be dynamic and socially constructed to take into account all voices and members especially those not ordinarily included. This deeper understanding is critical to move public health practice and research upstream to address structural and social determinants of health necessary for population-level reductions in health inequities [ 80 , 91 ].
Although there is widespread theoretical recognition of the importance of in-depth community participation in CHNAA, this has not been fully embraced in practice based on our review. Included studies reported community involvement in various stages of CHNAA with varying depth reflecting a continuum from no participation to extensive participation, in which most studies were located at the middle of the participation continuum. The literature review suggests while certain community stakeholders were engaged in the CHNAA process, most studies did not involve a broad range of stakeholders through adopting a full participation approach. One reason for this could be that for most studies conducted in the US, CHNAA was performed to comply with ACA requirements, which requires hospitals to incorporate inputs of the population served as part of the CHNAA process. Since community inputs as well as the process as a whole is not well-defined by these regulations [ 20 ], it seems that the majority of included US-based studies tried to meet legislative requirements by incorporating a minimum level of community and stakeholders’ participation in CHNAA process. In addition, the concept of community engagement in health services planning and implementation has evolved over recent years, from one-way consultative processes to bi-directional collaboration and shared leadership. Although undertaking an in-depth participatory approach through extensive participation of community stakeholders in CHNAAs may pose certain challenges for healthcare providers including requiring additional time and other resources to collaborate with community residents, we argue the benefits to this approach are important to improve health, as reported by some included studies [ 80 , 118 , 151 ].
A notable gap in the existing literature is the lack of long-term or longitudinal–assessment of CHNAA. The review showed that additional research into CHNAA implementation and outcomes is needed. Currently, there are limited data describing the impact of CHNAAs on health outcomes. However, there is ample evidence on different short-term impacts associated with CHNAA implementation, including, the development of health and social interventions, forming the new partnership, raising awareness on health issues, engaging policy-makers, and facilitating obtaining resources. In other words, it is unclear how CHNAA projects are linked directly to health outcomes. Furthermore, the mechanisms between the conduct and use of CHNAA remain largely unknown in the literature [ 152 , 153 ]. Clearly, not all CHNAA projects result in changes to policies or programmes, and conversely, many programme and policy decisions are made in the absence of CHNAA data [ 154 , 155 ]. Still, further research to understand these mechanisms and the long term impact of CHNAA is needed to support evidence of its use and value in addressing individual and population health needs.
This scoping review aimed to provide clarity and supplement the evidence on the key concepts, rationale, methods, tools and outcomes of community health needs and assets assessments (CHNAAs). Importantly, it highlights the need for holistic approaches to needs assessments to focus on physical, mental and social wellbeing, along with considering wider systems factors and structural challenges to individual and population health. Furthermore, the findings emphasize the inclusion of community assets in community health assessments, beginning foremost with community capabilities and knowledge. It is encouraging to see the use of pragmatic approaches including both qualitative and quantitative methods in CHNAA process in the literature. This will help to ensure that a robust and in-depth exploration of needs and assets is available to guide decision making. Although we recognize the challenges with providing consensus on definitions, processes and tools for CHNAA, we argue that more clarity is needed on the key considerations, steps and outcomes for this process across various settings. This study attempts to provide some theoretical insights and empirical information concerning the process, which hopefully will provide useful guidance to community organizations, policy- makers, health service providers and researchers seeking to develop and implement community health needs and assets assessment.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Institute of Medicne. The future of the public’s health in the 21st century: National Academy Press; 2003.
Fuller J, Bentley M, Shotton D. Use of community health needs assessment for regional planning in country South Australia. Aust J Rural Health. 2001;9(1):12–7. https://doi.org/10.1046/j.1440-1584.2001.00353.x .
Wright J, Williams R, Wilkinson JR. Development and importance of health needs assessment. BMJ. 1998;316(7140):1310–3. https://doi.org/10.1136/bmj.316.7140.1310 .
Wright J, Walley J. Assessing health needs in developing countries. BMJ. 1998;316(7147):1819–23. https://doi.org/10.1136/bmj.316.7147.1819 .
Jordan J, Dowswell T, Harrison S, Lilford RJ, Mort M. Health needs assessment: Whose priorities? Listening to users and the public. BMJ. 1998;316(7145):1668–70. https://doi.org/10.1136/bmj.316.7145.1668 .
Myers S, Stoto MA: Criteria for assessing the usefulness of community health assessments; a literature review. 2006. https://www.rand.org/pubs/technical_reports/TR314.html . Accessed 18 Nov 2020.
Centers for Disease Control and Prevention (CDC). Community needs assessment. Atlanta: GA.
Finifter DH, Jensen CJ, Wilson CE, Koenig BL. A comprehensive, multitiered, targeted community needs assessment model: methodology, dissemination, and implementation. Fam Community Health. 2005:293–306. https://doi.org/10.1097/00003727-200510000-00003 .
Stevens A, Gillam S. Needs assessment: from theory to practice. BMJ. 1998;316(7142):1448–52. https://doi.org/10.1136/bmj.316.7142.1448 .
Friedman DJ, Parrish RG. Is community health assessment worthwhile? J Public Health Manag Pract. 2009;15(1):3–9. https://doi.org/10.1097/01.PHH.0000342943.41080.ef .
Altschuld JW, Hung HL, Lee YF. Needs assessment and asset/capacity building: A promising development in practice. New Dir Eval. 2014;2014(144):89–103. https://doi.org/10.1002/ev.20105 .
Jackson KM, Pukys S, Castro A, Hermosura L, Mendez J, Vohra-Gupta S, et al. Using the transformative paradigm to conduct a mixed methods needs assessment of a marginalized community: Methodological lessons and implications. Eval Program Plann. 2018;66:111–9. https://doi.org/10.1016/j.evalprogplan.2017.09.010 .
Mathias KR, Mathias JM, Hill PC. An asset-focused health needs assessment in a rural community in North India. Asia Pac J Public Health. 2015;27(2):NP2623–34. https://doi.org/10.1177/1010539511421193 .
Kirk CM, Johnson-Hakim S, Anglin A, Connelly C. Putting the community back into community health needs assessments: Maximizing partnerships via community-based participatory research. Prog Community Health Partnersh. 2017;11(2):167–73. https://doi.org/10.1353/cpr.2017.0021 .
Coster G, Mays N, Scott C, Cumming J. The impact of health needs assessment and prioritisation on District Health Board planning in New Zealand. Int J Health Plann Manag. 2009;24(4):276–89. https://doi.org/10.1002/hpm.1011 .
Parry-Jones B, Soulsby J. Needs-led assessment: the challenges and the reality. Health Soc Care Community. 2001;9(6):414–28. https://doi.org/10.1046/j.0966-0410.2001.00316.x .
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evidence Implementation. 2015;13(3):141–6. https://doi.org/10.1097/XEB.0000000000000050 .
Anselma M, Chinapaw MJM, Altenburg TM. Determinants of child health behaviors in a disadvantaged area from a community perspective: A participatory needs assessment. Int J Environ Res Public Health. 2018;15(4):644. https://doi.org/10.3390/ijerph15040644 .
Berkley-Patton J, Thompson CB, Bradley-Ewing A, Marcie B, Booker A, Catley D, et al. Identifying health conditions, priorities, and relevant multilevel health promotion intervention strategies in African American churches: A faith community health needs assessment. Eval Program Plann. 2018;67:19. https://doi.org/10.1016/j.evalprogplan.2017.10.012 .
Bias TK, Abildso CG, Vasile E, Coffman J. The impact of community input in community health needs assessments. J Public Health Manag Pract. 2017;23:S29–33. https://doi.org/10.1097/PHH.0000000000000586 .
Cho S, Lee H, Yoon S, Kim Y, Levin P, Kim E. Community health needs assessment: a nurses’ global health project in Vietnam. Int Nurs Rev. 2018;65(4):505–14. https://doi.org/10.1111/inr.12443 .
Kapiriri L, Frithjof NorheimMD PDO. Whose priorities count? Comparison of community-identified health problems and Burden-of-Disease-assessed health priorities in a district in Uganda. Health Expect. 2002;5(1):55–62. https://doi.org/10.1046/j.1369-6513.2002.00161.x .
Li Y, Cao J, Lin H, Li D, Wang Y, He J. Community health needs assessment with precede-proceed model: a mixed methods study. BMC Health Serv Res. 2009;9(1):1–14. https://doi.org/10.1186/1472-6963-9-181 .
World Health Organization. Social Determinants of Health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 . Acessed 10 Oct 2022.
Smithies J, Adams L, Webster G, Beattie A. Community participation in health promotion: Health Education Authority London; 1990.
Jack K, Holt M. Community profiling as part of a health needs assessment. Nurs Stand. 2008;22(18):51–8. https://doi.org/10.7748/ns2008.01.22.18.51.c6311 .
Ahari SS, Habibzadeh S, Yousefi M, Amani F, Abdi R. Community based needs assessment in an urban area; A participatory action research project. BMC Public Health. 2012;12(1):1–8. https://doi.org/10.1186/1471-2458-12-161 .
Shin H, Lee SJ, Lee Y-n, Shon S. Community health needs assessment for a child health promotion program in Kyrgyzstan. Eval Program Plann. 2019;74:1–9. https://doi.org/10.1016/j.evalprogplan.2019.02.005 .
Birdwell SW, Calesaric H. Identifying Health Care Needs of Rural Ohio Citizens: An Evaluation of a Two-stage Methodology. J Rural Health. 1996;12(2):130–6. https://doi.org/10.1111/j.1748-0361.1996.tb00784.x .
Pepall E, Earnest J, James R. Understanding community perceptions of health and social needs in a rural Balinese village: results of a rapid participatory appraisal. Health Promot Int. 2007;22(1):44–52. https://doi.org/10.1093/heapro/dal042 .
Moore de Peralta A, Davis L, Brown K, Fuentes M, Falconer NS, Charles J, et al. Using Community-Engaged Research to Explore Social Determinants of Health in a Low-Resource Community in the Dominican Republic: A Community Health Assessment. Hisp Health Care Int. 2020;18(3):127–37. https://doi.org/10.1177/1540415319874812 .
Ake T, Diehr S, Ruffalo L, Farias E, Fitzgerald A, Good SD, et al. Needs assessment for creating a patient-centered, community-engaged health program for homeless pregnant women. J Patient Cent Res Rev. 2018;5(1):36. https://doi.org/10.17294/2330-0698.1591 .
Kiser T, Hulton L. Addressing health care needs in the homeless population: a new approach using participatory action research. SAGE Open. 2018;8(3):2158244018789750. https://doi.org/10.1177/2158244018789750 .
Schaffer MA, Mather S, Gustafson V. Service learning: A strategy for conducting a health needs assessment of the homeless. Health Care Poor Underserved. 2000;11(4):385–99. https://doi.org/10.1353/hpu.2010.0746 .
Kehn M, Ho P, Kroll T. Identifying the health service needs of homeless adults with physical disabilities. Public Health. 2013;127(8):785–7. https://doi.org/10.1016/j.puhe.2013.01.011 .
Sangalang CC, Ngouy S, Lau AS. Using community-based participatory research to identify health issues for Cambodian American youth. Fam Community Health. 2015;38(1):55. https://doi.org/10.1097/FCH.0000000000000056 .
Jeffery V, Ervin K. Responding to rural health needs through community participation: addressing the concerns of children and young adults. Aust Prim Health. 2011;17(2):125–30. https://doi.org/10.1071/PY10050 .
Harrison L, Scarinci I. Child health needs of rural Alabama Latino families. J Community Health Nurs. 2007;24(1):31–47. https://doi.org/10.1080/07370010709336584 .
Averill J. Keys to the puzzle: Recognizing strengths in a rural community. Public Health Nurs. 2003;20(6):449–55. https://doi.org/10.1046/j.1525-1446.2003.20605.x .
Din NC, Ghazali SE, Ibrahim N, Ahmad M, Said Z, Ghazali AR, et al. Health needs assessment of older people in an agricultural plantation. Int J Gerontol. 2014;8(3):120–6. https://doi.org/10.1016/j.ijge.2013.12.003 .
Nolin J, Wilburn ST, Wilburn KT, Weaver D. Health and social service needs of older adults: Implementing a community-based needs assessment. Eval Program Plann. 2006;29(3):217–26. https://doi.org/10.1016/j.evalprogplan.2006.06.003 .
Lee LL, Lin SH, Philp I. Health needs of older Aboriginal people in Taiwan: a community-based assessment using a multidimensional instrument. J Clin Nurs. 2015;24(17–18):2514–21. https://doi.org/10.1111/jocn.12842 .
Núñez AE, Robertson-James C, Reels S, Weingartner RM, Bungy BL. Conducting a needs assessment for women and girls using a gender analysis framework: The Philadelphia Ujima coalition for a healthier community experience. Womens Health Issues. 2012;22(6):e527–34. https://doi.org/10.1016/j.whi.2012.08.002 .
Urrutia RP, Merisier D, Small M, Urrutia E, Tinfo N, Walmer DK. Unmet health needs identified by Haitian women as priorities for attention: a qualitative study. Reprod Health Matters. 2012;20(39):93–103. https://doi.org/10.1016/s0968-8080(12)39602-x .
Zimmermann K, Khare MM, Wright C, Hasler A, Kerch S, Moehring P, et al. Application of a gender-based approach to conducting a community health assessment for rural women in Southern Illinois. Eval Program Plann. 2015;51:27–34. https://doi.org/10.1016/j.evalprogplan.2014.12.004 .
Dell EM, Erikson SL, Andrianirina E, Smith G. Women’s knowledge in Madagascar: A health needs assessment study. Global public health. 2012;7(1):29–41. https://doi.org/10.1080/17441692.2011.557083 .
Chhabra R, Teitelman N, Silver EJ, Raufman J, Bauman LJ. Vulnerability Multiplied: Health Needs Assessment of 13–18-Year-Old Female Orphan and Vulnerable Children in Kenya. World Med Health Policy. 2018;10(2):129–45. https://doi.org/10.1002/wmh3.267 .
Stepleman LM, Yohannan J, Scott SM, Titus LL, Walker J, Lopez EJ, et al. Health needs and experiences of a LGBT population in Georgia and South Carolina. Homosex. 2019;66(7):989–1013. https://doi.org/10.1080/00918369.2018.1490573 .
Wilson BD, Neubauer LC, Park A, Abuor P, Harper GW. The sexual health needs of sexual minority women in Western Kenya: An exploratory community assessment and public policy analysis. Glob Public Health. 2019;14(10):1495–508. https://doi.org/10.1080/17441692.2019.1611895 .
Zajac C, Godshall KC. Empowerment through accessibility: Community needs assessment data for LGBTQ communities. Soc Work Public Health. 2020;35(6):483–93. https://doi.org/10.1080/19371918.2020.1798322 .
Coleman JD, Irwin JA, Wilson RC, Miller HC. The South Carolina LGBT needs assessment: A descriptive overview. Homosex. 2014;61(8):1152–71. https://doi.org/10.1080/00918369.2014.872515 .
Bhimla A, Yap L, Lee M, Seals B, Aczon H, Ma GX. Addressing the health needs of high-risk Filipino Americans in the greater Philadelphia region. J Community Health. 2017;42(2):269–77. https://doi.org/10.1007/s10900-016-0252-0 .
Bopp M, Fallon EA, Bolton DJ, Kaczynski AT, Lukwago S, Brooks A. Conducting a Hispanic Health Needs Assessment in rural Kansas: Building the foundation for community action. Eval Program Plann. 2012;35(4):453–60. https://doi.org/10.1016/j.evalprogplan.2012.02.002 .
Burns JC, Teadt S, Bradley WW Sr, Shade GH Jr. Enhancing Adolescent and Young Adult Health Services! A Review of the Community Needs Assessment Process in an Urban Federally Qualified Health Center. Health Equity. 2020;4(1):218–24. https://doi.org/10.1089/heq.2019.0108 .
Corona R, Gonzalez T, Cohen R, Edwards C, Edmonds T. Richmond Latino needs assessment: A community-university partnership to identify health concerns and service needs for Latino youth. J Community Health. 2009;34(3):195–201. https://doi.org/10.1007/s10900-008-9140-6 .
Doyle E, Rager R, Bates D, Cooper C. Using community-based participatory research to assess health needs among migrant and seasonal farmworkers. Am J Health Educ. 2006;37(5):279–88. https://doi.org/10.1080/19325037.2006.10598916 .
Ghimire S, Cheong P, Sagadraca L, Chien L-C, Sy FS. A health needs assessment of the Filipino American community in the greater Las Vegas area. Health Equity. 2018;2(1):334–48. https://doi.org/10.1089/heq.2018.0042 .
Hebert-Beirne J, Felner JK, Castañeda Y, Cohen S. Enhancing themes and strengths assessment: leveraging academic-led qualitative inquiry in community health assessment to uncover roots of community health inequities. J Public Health Manag Pract. 2017;23(4):370–9. https://doi.org/10.1097/phh.0000000000000478 .
Hebert-Beirne J, Hernandez SG, Felner J, Schwiesow J, Mayer A, Rak K, et al. Using community-driven, participatory qualitative inquiry to discern nuanced community health needs and assets of Chicago’s La Villita, a Mexican immigrant neighborhood. J Community Health. 2018;43(4):775–86. https://doi.org/10.1007/s10900-018-0484-2 .
Hernandez SG, Genkova A, Castañeda Y, Alexander S, Hebert-Beirne J. Oral histories as critical qualitative inquiry in community health assessment. Health Educ Behav. 2017;44(5):705–15. https://doi.org/10.1177/1090198117728546 .
Lee S, Ma GX, Juon H-S, Martinez G, Hsu CE, Bawa J. Assessing the needs and guiding the future: findings from the health needs assessment in 13 Asian American communities of Maryland in the United States. J Immigr Minor Health. 2011;13(2):395–401. https://doi.org/10.1007/s10903-009-9310-3 .
Martinez IL, Carter-Pokras O. Assessing health concerns and barriers in a heterogeneous Latino community. J Health Care Poor Underserved. 2006;17(4):899–909. https://doi.org/10.1353/hpu.2006.0129 .
Mannix TR, Austin SD, Baayd JL, Simonsen SE. A community needs assessment of urban Utah American Indians and Alaska natives. J Community Health. 2018;43(6):1217–27. https://doi.org/10.1007/s10900-018-0542-9 .
Montano JJ, Acosta-Deprez V, Sinay T. Assessing the health care needs of Filipino Americans in greater Long Beach. Public Admin Manag. 2009;14(1):156.
Patel VV, Rajpathak S, Karasz A. Bangladeshi immigrants in New York City: a community based health needs assessment of a hard to reach population. J Immigr Minor Health. 2012;14(5):767–73. https://doi.org/10.1007/s10903-011-9555-5 .
Su D, Garg A, Wiens J, Meyer E, Cai G. Assessing health needs in African American churches: a mixed-methods study. J Relig Health. 2021;60(2):1179–97. https://doi.org/10.1007/s10943-019-00924-5 .
Suiter SV. Community health needs assessment and action planning in seven Dominican bateyes. Eval Program Plann. 2017;60:103–11. https://doi.org/10.1016/j.evalprogplan.2016.10.011 .
Thomas LR, Donovan DM, Sigo RL. Identifying community needs and resources in a Native community: A research partnership in the Pacific Northwest. Int J Ment Health Addict. 2010;8(2):362–73. https://doi.org/10.1007/s11469-009-9233-1 .
Weathers B, Barg FK, Bowman M, Briggs V, Delmoor E, Kumanyika S, et al. Using a mixed-methods approach to identify health concerns in an African American community. Am J Public Health. 2011;101(11):2087–92. https://doi.org/10.2105/AJPH.2010.191775 .
Dong X, Chang E, Wong E, Wong B, Skarupski KA, Simon MA. Assessing the health needs of Chinese older adults: Findings from a community-based participatory research study in Chicago's Chinatown. J Aging Res. 2010. https://doi.org/10.4061/2010/124246 .
Sarsour L, Tong VS, Jaber O, Talbi M, Julliard K. Health assessment of the Arab American community in southwest Brooklyn. J Community Health. 2010;35(6):653–9. https://doi.org/10.1007/s10900-010-9260-7 .
Thein K, Zaw KT, Teng R-E, Liang C, Julliard K. Health Needs in Brooklyn's Chinatown: A Pilot Assessment Using Rapid Participatory Appraisal. J Health Care Poor Underserved. 2009;20(2):378–94. https://doi.org/10.1353/hpu.0.0140 .
Careyva BA, Hamadani R, Friel T, Coyne CA. A social needs assessment tool for an urban Latino population. J Community Health. 2018;43(1):137–45. https://doi.org/10.1007/s10900-017-0396-6 .
Johnson CV, Bartgis J, Worley JA, Hellman CM, Burkhart R. Urban Indian voices: a community-based participatory research health and needs assessment. Am Indian Alsk Native Mentl Health Res. 2010;17(1):49–70. https://doi.org/10.5820/aian.1701.2010.49 .
Puertas B, Schlesser M. Assessing community health among indigenous populations in Ecuador with a participatory approach: implications for health reform. J Community Health. 2001;26(2):133–47. https://doi.org/10.1023/a:1005281314274 .
Miller K, Yost B, Abbott C, Thompson Buckland S, Dlugi E, Adams Z, et al. Health needs assessment of five Pennsylvania Plain populations. Int J Environ Res Public Health. 2019;16(13):2378. https://doi.org/10.3390/ijerph16132378 .
Tendulkar SA, Hamilton RC, Chu C, Arsenault L, Duffy K, Huynh V, et al. Investigating the myth of the “model minority”: a participatory community health assessment of Chinese and Vietnamese adults. J Immigr Minor Health. 2012;14(5):850–7. https://doi.org/10.1007/s10903-011-9517-y .
Peak T, Gast J, Ahlstrom D. A needs assessment of Latino men’s health concerns. Am J Mens Health. 2010;4(1):22–32. https://doi.org/10.1177/1557988308327051 .
Brock KE, Allen KE, Barton C, Shapiro R, Weintraub B, Wasilewski-Masker K, et al. A Methodologic Approach to Conducting a Statewide Community Needs Assessment of Pediatric Palliative Care and Hospice Resources. J Pain Symptom Manag. 2020;60(3):531–8. e538. https://doi.org/10.1016/j.jpainsymman.2020.04.004 .
Franz BA, Skinner D, Murphy JW. Defining “Community” in community health evaluation: perspectives from a sample of nonprofit Appalachian hospitals. Am J Eval. 2018;39(2):237–56. https://doi.org/10.1177/1098214017722857 .
Clark MJ, Cary S, Diemert G, Ceballos R, Sifuentes M, Atteberry I, et al. Involving communities in community assessment. Public Health Nurs. 2003;20(6):456–63. https://doi.org/10.1046/j.1525-1446.2003.20606.x .
Van Gelderen SA, Krumwiede KA, Krumwiede NK, Fenske C. Trialing the community-based collaborative action research framework: supporting rural health through a community health needs assessment. Health Promot Pract. 2018;19(5):673–83. https://doi.org/10.1177/1524839917754043 .
Goldman KD, Schmalz KJ. “Accentuate the positive!” using an asset-mapping tool as part of a community-health needs assessment. Health Promot Pract. 2005;6(2):125–8. https://doi.org/10.1177/1524839904273344 .
Sharpe PA, Greaney ML, Lee PR, Royce SW. Assets-oriented community assessment. Public Health Rep. 2000;115(2–3):205. https://doi.org/10.1093/phr/115.2.205 .
Mathias K, Rawat M, Thompson A, Gaitonde R, Jain S. Exploring community mental health systems–A participatory health needs and assets assessment in the Yamuna valley, North India. Int J Health Policy Manag. 2020. https://doi.org/10.34172/ijhpm.2020.222 .
deValpine MG, Trull LH. Health Equity in Community Assessments: A Participatory Approach in Rural Virginia. SAGE Open. 2019;9(1):2158244019838925. https://doi.org/10.1177/2158244019838925 .
Lewis H, Rudolph M, White L. Rapid appraisal of the health promotion needs of the Hillbrow Community, South Africa. Int J Healthc Technol Manag. 2003;5(1–2):20–33. https://doi.org/10.1504/IJHTM.2003.003338 .
Talmage C, Mercado M, Yoder G, Hamm K, Wolfersteig W. Critiquing Indicators of Community Strengths in Community Health Needs Assessments. Int J Community Well-Being. 2021:1–22. https://doi.org/10.1007/s42413-020-00106-2 .
Idali Torres M. Assessing health in an urban neighborhood: community process, data results and implications for practice. J Community Health. 1998;23(3):211–26. https://doi.org/10.1023/a:1018720515644 .
Garrettson M, Walline V, Heisler J, Townsend J. New medical school engages rural communities to conduct regional health assessment. Fam Med. 2010;42(10):693.
Cain CL, Orionzi D, O’Brien M, Trahan L. The power of community voices for enhancing community health needs assessments. Health Promot Pract. 2017;18(3):437–43. https://doi.org/10.1177/1524839916634404 .
Grant CG, Ramos R, Davis JL, Green BL. Community health needs assessment: a pathway to the future and a vision for leaders. Health Care Manag (Frederick). 2015;34(2):147–56. https://doi.org/10.1097/hcm.0000000000000057 .
Robinson A, Cherry TS, Elliott M, Davis M, Bagwell G. Leveraging university-community partnerships in rural Georgia: A community health needs assessment template for hospitals. J Ga Public Health Assoc. 2016:365–72. https://doi.org/10.21633/JGPHA.5.409 .
Alfano-Sobsey E, Ledford SL, Decosimo K, Horney JA. Community health needs assessment in Wake County, North Carolina: partnership of public health, hospitals, academia, and other stakeholders. N C Med J. 2014;75(6):376–83. https://doi.org/10.18043/ncm.75.6.376 .
Waling A, Fildes D. ‘Don't fix what ain’t broke’: evaluating the effectiveness of a Men's Shed in inner-regional A ustralia. Health Soc Care Community. 2017;25(2):758–68. https://doi.org/10.1111/hsc.12365 .
Witten NA, Orr MP, Maskarinec GG. Medical School Hotline: An Online, Quantitative Community Health Needs Assessment of Hale ‘iwa and Waialua, O ‘ahu, Hawai ‘i. H Hawaii J Health Soc Welf. 2020;79(10):306.
Woodyard CD, Przybyla S, Hallam JS. A community health needs assessment using principles of community-based participatory research in a Mississippi Delta community: a novel methodological approach. Community Dev. 2015;46(2):84–99. https://doi.org/10.1080/15575330.2015.1006240 .
O’Kelly C, Cullen W, O’Kelly S, O’Kelly F, Bury G. A primary care-based health needs assessment in inner city Dublin. Ir J Med Sci. 2010;179(3):399–403. https://doi.org/10.1007/s11845-010-0483-5 .
Knox S, Chapman P, Your health—your say. A case study of community involvement in a community health needs assessment project in a regional city of Australia. Cities. 1995;12(2):111–4. https://doi.org/10.1016/0264-2751(95)00011-a .
Murray SA, Tapson J, Turnbull L, McCallum J, Little A. Listening to local voices: adapting rapid appraisal to assess health and social needs in general practice. BMJ. 1994;308(6930):698–700. https://doi.org/10.1136/bmj.308.6930.698 .
Stanley SA, Stein DS. Health Watch 2000: community health assessment in south central Ohio. J Community Health Nurs. 1998;15(4):225–36. https://doi.org/10.1207/s15327655jchn1504_4 .
Ying L, Daikun L, Jia H, Kai S, HongHong L, Hu Z. Assessment of community health needs of Chongqing residents. a qualitative study. Mil Med Res. 2008;23(5):289–99. https://doi.org/10.1016/S1000-1948(08)60056-8 .
Kwan K, Do-Reynoso V, Zarate-Gonzalez G, Goldman-Mellor S. Development and implementation of a community health survey for public health accreditation: Case study from a rural county in California. Eval Program Plann. 2018;67:47–52. https://doi.org/10.1016/j.evalprogplan.2017.11.004 .
Green S, Parkinson L, Bonevski B, Considine R. Community health needs assessment for health service planning: realising consumer participation in the health service setting. Health Promot J Austr. 2004;15(2):142–9. https://doi.org/10.1071/HE04142 .
Horne M, Costello J. A public health approach to health needs assessment at the interface of primary care and community development: findings from an action research study. Prim Health Care Res Dev. 2003;4(4):340–52. https://doi.org/10.1191/1463423603pc173oa .
Lundeen SP. Health needs of a suburban community: a nursing assessment approach. J Community Health Nurs. 1992;9(4):235–44. https://doi.org/10.1207/s15327655jchn0904_5 .
Jordan J, Wright J. Making sense of health needs assessment. Br Gen Pract. 1997;47(424):695.
Hensher M, Fulop N. The influence of health needs assessment on health care decision-making in London health authorities. J Health Serv Policy. 1999;4(2):90–5. https://doi.org/10.1177/135581969900400206 .
Asadi-Lari M, Farshad A, Assaei S, Mahdavi MV, Akbari M, Ameri A, et al. Applying a basic development needs approach for sustainable and integrated community development in less-developed areas: report of ongoing Iranian experience. Public Health. 2005;119(6):474–82. https://doi.org/10.1016/j.puhe.2004.08.014 .
Akintobi TH, Lockamy E, Goodin L, Hernandez ND, Slocumb T, Blumenthal D, et al. Processes and outcomes of a community-based participatory research-driven health needs assessment: a tool for moving health disparity reporting to evidence-based action. Prog Community Health Partnersh. 2018;12(1 Suppl):139. https://doi.org/10.1353/cpr.2018.0029 .
Yoo IY, Cho WJ, Chae SM, Kim MJ. Community health service needs assessment in Korea using OMAHA Classification System. Int J Nurs Stud. 2004;41(6):697–702. https://doi.org/10.1016/j.ijnurstu.2004.02.007 .
Louw J, Carolissen R. Community health needs, community participation, and evaluation research. Eval Program Plann. 1995;18(4):365–9.
Plescia M, Koontz S, Laurent S. Community assessment in a vertically integrated health care system. Am J Public Health. 2001;91(5):811. https://doi.org/10.2105/AJPH.91.5.811 .
Sampson G, Gearin KJM, Boe M. A rural local health department–hospital collaborative for a countywide community health assessment. J Public Health Manag Pract. 2015;21(1):23–30. https://doi.org/10.1097/phh.0000000000000088 .
Vyas AN, Chaudhary N, Ramiah K, Landry M. Addressing a Growing Community’s Health Needs: Project SAHNA (South Asian Health Needs Assessment). J Immigr Minor Health. 2013;15(3):577–83. https://doi.org/10.1007/s10903-012-9655-x .
Van Rie A, West N, Schwartz S, Mutunga L, Hanrahan C, Ncayiyana J, et al. The unmet needs and health priorities of the urban poor: Generating the evidence base for urban community health worker programmes in South Afric. S Afr Med J. 2018;108(9). https://doi.org/10.7196/SAMJ.2018.v108i9.13054 .
Dennis MK, Momper SL. An urban American Indian health clinic's response to a community needs assessment. Am Indian Alsk Native Ment Health Res. 2016;23(5). https://doi.org/10.5820/aian.2305.2016.15 .
Schutte DL, Goris ED, Rivard JL, Schutte BC, Committee CCRA. Community Health Needs Assessment in a Rural Setting. Foundation for a Community–Academic Partnership. J High Educ Outreach Engagem. 2016;20(2):85–108.
Velonis AJ, Molnar A, Lee-Foon N, Rahim A, Boushel M, O’Campo P. “One program that could improve health in this neighbourhood is _?” using concept mapping to engage communities as part of a health and human services needs assessment. BMC Health Serv Res. 2018;18(1):1–12. https://doi.org/10.1186/s12913-018-2936-x .
Torres Stone RA, Cardemil EV, Keefe K, Bik P, Dyer Z, Clark KE. A community mental health needs assessment of a racially and ethnically diverse population in New England: Narratives from community stakeholders. Community Ment Health J. 2020;56(5):947–58. https://doi.org/10.1007/s10597-020-00562-2 .
Agrusti T, Bohn J, Dunn E, Bell C, Ziegler A. The story so far: a mixed-methods evaluation of county-level behavioral health needs, policies, and programs. Soc Work Ment Health. 2020;18(3):257–73. https://doi.org/10.1080/15332985.2020.1720889 .
Palmer CA. Rapid appraisal of needs in reproductive health care in southern Sudan: qualitative study. BMJ. 1999;319(7212):743–8. https://doi.org/10.1136/bmj.319.7212.743 .
Lazenbatt A, Lynch U, O'Neill E. Revealing the hidden ‘troubles’ in Northern Ireland: the role of participatory rapid appraisal. Health Educ Res. 2001;16(5):567–78. https://doi.org/10.1093/her/16.5.567 .
Kingery FP, Naanyu V, Allen W, Patel P. Photovoice in Kenya: Using a community-based participatory research method to identify health needs. Qual Health Res. 2016;26(1):92–104. https://doi.org/10.1177/1049732315617738 .
Sabin AV, Levin PF. The Journey to Meet Emerging Community Benefit Requirements in a Rural Hospital: A Case Study. Online J Issues Nurs. 2016;21(1). https://doi.org/10.3912/OJIN.Vol21No01PPT01 .
Lightfoot AF, De Marco MM, Dendas RC, Jackson MR, Meehan EF. Engaging underserved populations in Affordable Care Act-required needs assessments. J Health Care Poor Underserved. 2014;25(1):11–8. https://doi.org/10.1353/hpu.2014.0060 .
Amendola MG, Nazario N, Sanchez V. Using CBPR to assess client needs at a social service agency. Public Health Nurs. 2016;33(2):167–75. https://doi.org/10.1111/phn.12204 .
Harmon BE, Pichon LC, Powell TW, Rugless F, McCann L, Minor LL, et al. Developing a Congregational Health Needs Assessment: Lessons Learned from Using a Participatory Research Approach. Prog Community Health Partnersh. 2021;15(1):47–58. https://doi.org/10.1353/cpr.2021.0004 .
Mulvihill BA, Pass MA, Miller TM, Mulvihill FX, Klerman LV. Collaborative needs assessment and systems development in Alabama: Process and products. Am J Prev Med. 1996;12(4):14–9.
Santilli A, Carroll-Scott A, Ickovics JR. Applying community organizing principles to assess health needs in New Haven, Connecticut. Am J Public Health. 2016;106(5):841–7. https://doi.org/10.2105/ajph.2016.303050 .
Milaat W, Bani I, Aqeely H, Makeen A, Salih A, Alnagaar M. Jazan Health needs assessment: a key informant approach. J Public Health Med. 2007;6:105–10.
Kulig JC, Wilde I. Collaboration between communities and universities: Completion of a community needs assessment. Public Health Nurs. 1996;13(2):112–9. https://doi.org/10.1111/j.1525-1446.1996.tb00228.x .
Running A, Martin K, Tolle LW. An innovative model for conducting a participatory community health assessment. J Community Health Nurs. 2007;24(4):203–13. https://doi.org/10.1080/07370010701645869 .
Smith SM, Long J, Deady J, O'Keeffe F, Handy D, O'Dowd T. Adapting developing country epidemiological assessment techniques to improve the quality of health needs assessments in developed countries. BMC Health Serv Res. 2005;5(1):1–7. https://doi.org/10.1186/1472-6963-5-32 .
Wood EA, Chapman KS, Beau de Rochars VM, Mckune SL. Community-based health needs assessment in Léogâne and Gressier, Haiti: six years post-earthquake. J Int Humanit Action. 2017;2(1):1–8. https://doi.org/10.1186/s41018-017-0026-z .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. A mixed-methods approach to understanding community participation in community health needs assessments. J Public Health Manag Pract. 2017;23(2):112–21. https://doi.org/10.1097/PHH.0000000000000362 .
Lillie-Blanton M, Hoffman SC. Conducting an assessment of health needs and resources in a racial/ethnic minority community. Health Serv Res. 1995;30(1 Pt 2):225.
Irani P, Bohn C, Halasan C, Landen M, McCusker D. Community health assessment: driving the need for current, easily accessible population health data. J Public Health Manag Pract. 2006;12(2):113–8. https://doi.org/10.1097/00124784-200603000-00002 .
Alberti P. Community health needs assessments: filling data gaps for population health research and management. EGEMS. 2014;2(4). https://doi.org/10.13063/2327-9214.1174 .
Skinner D, Franz B, Kelleher K. What challenges do nonprofit hospitals face in taking on community health needs assessments? A qualitative study from Appalachian Ohio. J Rural Health. 2018;34(2):182–92. https://doi.org/10.1111/jrh.12246 .
Stoto MA, Davis MV, Atkins A. Making better use of population health data for community health needs assessments. EGEMs. 2019;7(1). https://doi.org/10.5334/egems.305 .
Smith LU, Burdine JN. Community health assessment opportunities and challenges in the 21st century: Implications for professional development. J Public Health Manag Pract. 2017;23:S63–4. https://doi.org/10.1097/PHH.0000000000000601 .
Hawe P. Needs assessment must become more change-focused. Aust N Z J Public Health. 1996;20(5):473–8. https://doi.org/10.1111/j.1467-842x.1996.tb01624.x .
Jordan J, Wright J, Wilkinson J, Williams R. Assessing local health needs in primary care: understanding and experience in three English districts. Qual Health Care. 1998;7(2):83–9. https://doi.org/10.1136/qshc.7.2.83 .
Curtis DC. Evaluation of community health assessment in Kansas. J Public Health Manag Pract. 2002:20–5. https://doi.org/10.1097/00124784-200207000-00005 .
Kim S, Flaskerud JH, Koniak-Griffin D, Dixon EL. Using community-partnered participatory research to address health disparities in a Latino community. J Prof Nurs. 2005;21(4):199–209. https://doi.org/10.1016/j.profnurs.2005.05.005 .
Crossley M. Tax-exempt hospitals, community health needs and addressing disparities. Howard Law J. 2011;55:687.
Schifferdecker KE, Bazos DA, Sutherland KA, LaFave LRA, Fedrizzi R, Hoebeke J. A review of tools to assist hospitals in meeting community health assessment and implementation strategy requirements. J Healthc Manag. 2016;61(1):44.
Becker KL. Conducting community health needs assessments in rural communities: Lessons learned. Health Promot Pract. 2015;16(1):15–9. https://doi.org/10.1177/1524839914555887 .
Pepall E, James R, Earnest J. Guidelines for conducting rapid participatory appraisals of community health needs in developing countries: experience from Tulikup, Bali. Asia Pac J Public Health. 2006;18(3):42–8. https://doi.org/10.1177/10105395060180030801 .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. Community health needs assessment: potential for population health improvement. Popul Health Manag. 2016;19(3):178–86. https://doi.org/10.1089/pop.2015.0075 .
Solet D, Ciske S, Gaonkar R, Horsley K, McNees M, Nandi P, et al. Effective community health assessments in King County, Washington. J Public Health Manag Pract. 2009;15(1):33–40. https://doi.org/10.1097/PHH.0b013e3181903c11 .
Spice C, Snyder K. Reviewing self-reported impacts of community health assessment in local health jurisdictions. J Public Health Manag Pract. 2009;15(1):18–23. https://doi.org/10.1097/PHH.0b013e3181903c57 .
Diaz HJ-M, Ainsworth D, Schmidtlein MC. Funding priorities: data-driven approach for prioritizing community health needs in vulnerable communities. Health Promot Pract. 2019;20(4):616–23. https://doi.org/10.1177/1524839918771977 .
Franz B, Cronin CE, Singh S. Are nonprofit hospitals addressing the most critical community health needs that they identify in their community health needs assessments? J Public Health Manag Pract. 2021;27(1):80–7. https://doi.org/10.1097/phh.0000000000001034 .
Cramer GR, Singh SR, Flaherty S, Young GJ. The progress of US hospitals in addressing community health needs. Am J Public Health. 2017;107(2):255–61. https://doi.org/10.2105/AJPH.2016.303570 .
Kazda MJ, Beel ER, Villegas D, Martinez JG, Patel N, Migala W. Methodological complexities and the use of GIS in conducting a community needs assessment of a large US municipality. J Community Health. 2009;34(3):210–5. https://doi.org/10.1007/s10900-008-9143-3 .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D. Nonprofit hospitals’ approach to community health needs assessment. Am J Public Health. 2015;105(3):e103–13. https://doi.org/10.2105/ajph.2014.302286 .
Vance RA, Basta TB, Bute JJ, Denham SA. Identifying the health needs in rural Appalachian Ohio: Outcomes of a rural community-academic partnership. Am J Health Sci. 2012;3(2):115–24. https://doi.org/10.19030/ajhs.v3i2.6942 .
Bias T, Abildso C, Sarkees E. The Importance of Individual-Site and System-Wide Community Health Needs Assessments. Front Public Health. 2020;20. https://doi.org/10.3389/fpubh.2020.00020 .
Billings JR, Cowley S. Approaches to community needs assessment: a literature review. J Adv Nurs. 1995;22(4):721–30. https://doi.org/10.1046/j.1365-2648.1995.22040721.x .
Brazil K, Anderson M. Assessing health service needs: Tools for health planning. HealthC Manage Forum. 1996:22–7. https://doi.org/10.1016/S0840-4704(10)60940-4 .
Campbell S. Assessing community healthcare needs: lessons from Africa. Nurs Stand. 2001;15(47):41. https://doi.org/10.7748/ns2001.08.15.47.41.c3070 .
Carlton EL, Singh SR. Joint community health needs assessments as a path for coordinating community-wide health improvement efforts between hospitals and local health departments. Am J Public Health. 2018;108(5):676–82. https://doi.org/10.2105/ajph.2018.304339 .
Declercq ER, Bichell TJV, Center JK. Population-based needs assessment: bringing public health to midwifery practice. J Nurse Midwifery. 1997;42(6):478–88. https://doi.org/10.1016/s0091-2182(97)00081-5 .
Evans-Agnew R, Reyes D, Primomo J, Meyer K, Matlock-Hightower C. Community health needs assessments: Expanding the boundaries of nursing education in population health. Public Health Nurs. 2017;34(1):69–77. https://doi.org/10.1111/phn.12298 .
Guareschi PA, Jovchelovitch S. Participation, health and the development of community resources in Southern Brazil. J Health Psychol. 2004;9(2):311–22. https://doi.org/10.1177/1359105304040896 .
Holakouie NK, Ahmadvand A, Ahmadnezhad E, Alami A. A community assessment model appropriate for the Iranian community. Iran J Public Health. 2014;43(3):323.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173–202. https://doi.org/10.1146/annurev.publhealth.19.1.173 .
King CJ, Roach JL. Community health needs assessments: a framework for America’s hospitals. Popul Health Manag. 2016;19(2):78–80. https://doi.org/10.1089/pop.2015.0053 .
Misra R, Ballard D. Community needs and strengths assessments as an active learning project. J Sch Health. 2003;73(7):269–71. https://doi.org/10.1111/j.1746-1561.2003.tb06577.x .
Powell RE, Doty AM, Rising KL, Karp DN, Baehr A, Carr BG. A content analysis of nonprofit hospital community health needs assessments and community benefit implementation strategies in Philadelphia. J Public Health Manag Pract. 2018;24(4):326–34. https://doi.org/10.1097/phh.0000000000000621 .
Reece SM. Community analysis for health planning: strategies for primary care practitioners. The. Nurse Pract. 1998;23(10):46 49, 53-46 passim.
Stoto MA, Straus SG, Bohn C, Irani P. A web-based tool for assessing and improving the usefulness of community health assessments. J Public Health Manag Pract. 2009;15(1):10–7. https://doi.org/10.1097/01.PHH.0000342944.48703.21 .
Wetta RE, Pezzino G, LaClair B, Orr S, Brown MB. Voices across Kansas: community health assessment and improvement efforts among local health departments. J Public Health Manag Pract. 2014;20(1):39–42. https://doi.org/10.1097/phh.0b013e3182a9572a .
We acknowledge contribution of the research assistants helped with data extraction.
This work was funded by department of UHC Life course/Integrated Health Services (IHS), World Health Organization (WHO) headquarter (HQ). ZA received the research grant. The authors HR, AS, and SE from WHO commissioned the study, contributed to the direction of the work, and commented on the drafts.
Department of Universal Health Coverage/Health Systems (UHS), World Health Organization, Regional Office for the Eastern Mediterranean, Cairo, Egypt
Hamid Ravaghi
Department of Integrated Health Services (IHS), World Health Organization, Headquarters, Geneva, Switzerland
Ann-Lise Guisset
Department of Healthier Populations (DHP), World Health Organization, Regional Office of Eastern Mediterranean Region, Cairo, Egypt
Samar Elfeky
Center for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Naima Nasir
National library and Archives of Iran, Tehran, Iran
Sedigheh Khani
National Institute of Health Research (NIHR), Tehran University of Medical Sciences, Tehran (TUMS), Tehran, Iran
Elham Ahmadnezhad
Zhaleh Abdi
AG, HR and SE conceived the study and participated in its design. SK conducted the literature search and prepared the search results for analysis. NN developed the study framework, the data abstraction forms and the manuscript outline. The literature was analysed by ZA, EA and NN under the supervision of HR and AG. ZA drafted the final version of the manuscript and HR, NN, AG and SE reviewed it. All authors read and approved the final manuscript.
Correspondence to Zhaleh Abdi .
Competing interests.
The authors have no competing interests. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the World Health Organization (WHO).
Supplementary Information
Additional file 1..
PubMed database search strategy.
Additional file 2.
Content of the extraction forms.
Additional file 3.
List of included empirical papers [ 156 – 159 ].
Additional file 4.
List of included non-empirical papers [ 160 -– 175 ] .
Additional file 5.
Health indicators collected by community health assessment surveys.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Ravaghi, H., Guisset, AL., Elfeky, S. et al. A scoping review of community health needs and assets assessment: concepts, rationale, tools and uses. BMC Health Serv Res 23 , 44 (2023). https://doi.org/10.1186/s12913-022-08983-3
Received : 20 May 2022
Accepted : 19 December 2022
Published : 17 January 2023
DOI : https://doi.org/10.1186/s12913-022-08983-3
- Health Needs Assessment
- Needs Assessment
- Assets Assessment
- Population Health
- Scoping Review
BMC Health Services Research
ISSN: 1472-6963
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Program Portfolio
Exposure Assessment Program
- The Exposure Assessment Program provides national and international leadership in the development and use of effective exposure assessment strategies and tools to prevent work-related illness and injury.
- The program promotes the use of 21st century exposure assessment sensors, methods, and processes to protect worker safety, health, well-being, and productivity.
Exposure Assessment is the multi-disciplinary field that identifies and characterizes workplace exposures, develops estimates of exposure for exposure-response and risk assessment studies, and evaluates the significance of exposures and effectiveness of intervention strategies.
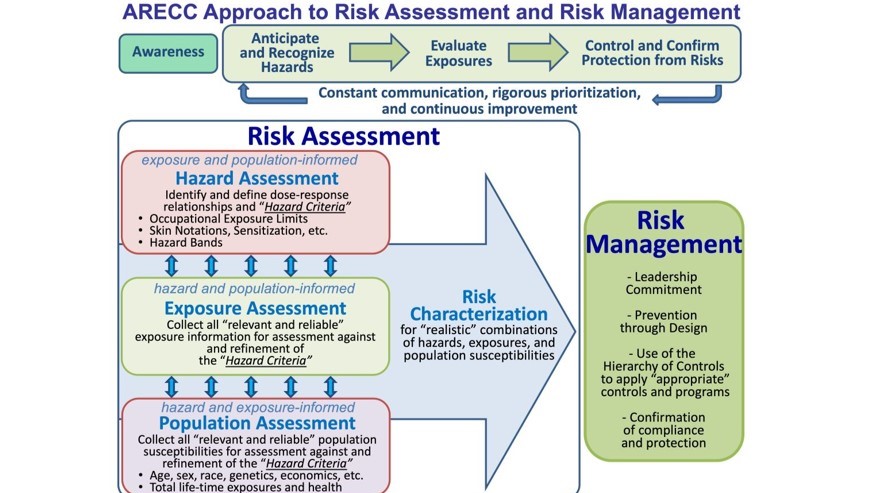
To Learn More
Occupational exposure assessment enables effective anticipation, recognition, evaluation, control, and confirmation of protection from workplace hazards. At each stage, health professionals consider the available information and develop a course of action that may include continuing along the original exposure assessment process, determining that no further action is required, performing additional hazard identification, refining the exposure assessment, or improving or adding engineering and/or administrative controls.
Program priorities
The EXA Program has selected research priorities on the basis of burden, need, and impact and collaborated with other NIOSH research programs to write the research goals in the NIOSH Strategic Plan for FYs 2019-2026 . Priority areas include (but are not limited to):
- Better understanding pesticide exposures and chronic kidney disease of unknown etiology among agriculture and forestry workers.
- Potentially carcinogenic chemicals that are new or increasingly used in the manufacturing sector, including nanomaterials, flame retardant chemicals, bisphenol A (BPA) and other plasticizers, and per- and polyfluoroalkyl substances (PFAS).
- Measuring known or suspected lung carcinogens in the mining sector, such as silica, elongated mineral particles, and radon.
- Direct reading instruments for potential carcinogens left on fire fighters' gear after cleaning.
- Different workplace factors such as workplace stress, heat stress, and shiftwork and how they are interrelated with cardiovascular disease causation and progression among workers in the services sector.
- Hazardous dermal exposures among agriculture and oil and gas extraction industry workers.
What we've accomplished
In 2022-2023, the Program:
- Completed an exposure study on carcinogenic exposures for refined coal tar sealant workers.
- Completed studies to determine the effectiveness of controls to protect workers from SARS-CoV-2, the virus that causes COVID-19, including the use of physical barriers in customer-facing industries and ventilation control strategies in school buses .
- Developed a technical report that provides exposure assessment sampling and analytical methods to evaluate occupational risk for engineered nanomaterials (ENM). Increased ENM production, combined with widespread usage, has increased the likelihood of occupational exposure.
- Developed a new NMAM Chapter on Surface Sampling Strategies and Methods and published updated NMAM Chapters on Biological Monitoring and Fiber Characterization .
- Published new methods for the measurement of antimicrobial peracetic acid (PAA) using colorimetry and mass spectrometry and for its controlled laboratory generation to aid in evaluation of samplers for peracetic acid collection. PAA is most used in the food and beverage, healthcare, and sanitation industries and can irritate respiratory tract, skin, and eyes.
- Hosted an internal symposium among NIOSH exposure assessment scientists to discuss future exposure assessment areas of research.
- Pilot tested a data collection tool to assess and document impacts and research uptake of NIOSH exposure assessment research on Bisphenol A (BPA) and firefighting exposures .
What's ahead
In the future, the Program aims to:
- Conduct worker exposure and health assessments in manufacturing workers, service sector workers, and firefighters exposed to per- and polyfluoroalkyl substances ( PFAS ).
- Develop new methods and exposure assessment approaches for PFAS in stain-resistant and moisture-repellent textiles, firefighting foam, medical devices, and construction materials.
- Publish a new NMAM method for assessing exposures to Bisphenol A and Bisphenol S.
More information on specific workplace safety and health topics and useful resources can be found on the following pages:
- NIOSH Manual of Analytical Methods (NMAM) 5th Edition
- NIOSH Center for Direct Reading and Technologies
- Health Hazard Evaluations
National Institute for Occupational Safety and Health (NIOSH)
The Occupational Safety and Health Act of 1970 established NIOSH as a research agency focused on the study of worker safety and health, and empowering employers and workers to create safe and healthy workplaces.
NIOSH Research Programs
Health assessment is a process involving systematic collection and analysis of health-related information on patients for use by patients, clinicians, and health care ... Much of the research on health assessments has focused primarily on their use and application in work settings. In these settings, successful use of health assessments ...
Health is a central feature for achieving a high quality of life. Health assessment has been a major concern for researchers and scholars, and there is a huge amount of literature on the theoretical and technical aspects of this challenge. Amartya Sen's Capability Approach (CA) offers a framework to assess human well-being (Anand, Hunter ...
The Colorado Research Network's Patient Advisory Council created this definition of health assessments for patients. What is a health assessment? A health assessment is a set of questions, answered by patients, that asks about personal behaviors, risks, life-changing events, health goals and priorities, and overall health.
Assessing patients, determining whether their conditions are stable or unstable, and defining care needs are important tasks for ECNs. 10 Failure to assess patients according to their individual care needs may lead to undesired consequences, such as incomplete nursing care and adverse health events. 13 In Sweden, patient assessment generally focuses on patients' physical and biomedical ...
DEFINITION OF HEALTH IMPACT ASSESSMENT. The committee proposes on the basis of its review the following adaptation of the current working definition of the International Association of Impact Assessment (Quigley et al. 2006) as a technical definition of HIA:HIA is a systematic process that uses an array of data sources and analytic methods and considers input from stakeholders to determine the ...
Accepting this responsibility requires an understanding of how to assess the health needs of a population. The GP curriculum and assessing health needs. Clinical statement 3.01: Healthy people: promoting health and preventing disease states that GPs have a key role in promoting health and preventing disease.
The ability to effectively measure health-related quality-of-life longitudinally is central to describing the impacts of disease, treatment, or other insults, including normal aging, upon the patient. Over the last two decades, assessment of patient health status has undergone a dramatic paradigm shift, evolving from a predominant reliance on biochemical and physical measurements, such as ...
The Public Health Accreditation Board defines community health assessment (or CHA) as a comprehensive picture of a community's current health status, factors contributing to higher health risks or poorer health outcomes, and community resources available to improve health.Community health assessments are comprised of data and information from multiple sources, which describe the community's ...
The definition of health equity developed during the establishment of ... systematic efforts to address public health problems based on the results of community health assessment activities and the ... and language groups as well as medical vulnerability. The SVI "can be used to apply a health equity lens to research, strategic planning ...
Definition of needs. ... Burkhart R. Urban Indian voices: a community-based participatory research health and needs assessment. Am Indian Alsk Native Mentl Health Res. 2010; 17 (1):49-70. doi: 10.5820/aian.1701.2010.49. [Google Scholar] 75. Puertas B, Schlesser M. Assessing community health among indigenous populations in Ecuador with a ...
A community health assessment, also known as community health needs assessment, refers to a state, tribal, local, or territorial health assessment that identifies key health needs and issues through systematic, comprehensive data collection and analysis.A community health improvement plan is a long-term, systematic effort to address public health problems based on the results of community ...
Community health assessments use such principles as. Multisector collaborations that support shared ownership of all phases of community health improvement, including assessment, planning, investment, implementation, and evaluation. Proactive, broad, and diverse community engagement to improve results. A definition of community that encompasses ...
A community health needs assessment is not a one-off activity but a developmental process that is added to and amended over time. It is not an end in itself but a way of using information to plan health care and public health programmes in the future. The steps of community health needs assessment are as follows.
Health Impact Assessment (HIA) is a practical approach used to judge the potential health effects of a proposed policy, programme or project on a population, particularly on vulnerable or disadvantaged groups. Recommendations are produced for decision-makers and stakeholders, with the aim of maximizing the proposal's positive health effects and minimizing its negative health effects.
Community health assessments (CHAs) provide information for problem and asset identification and policy formulation, implementation, and evaluation. CHAs also help measure how well a public health system is fulfilling its assurance function. 1,2. A CHA should be part of an ongoing broader community health improvement process.
An overview of rural health research, needs assessments, and program evaluation, with tools and resources to support these activities. ... Definitions for Health Policy and Research, discusses the importance of using an appropriate rural definition to develop research findings that offer accurate conclusions. The three key considerations the ...
This health assessment tool is based on the perspective of three-dimensional health definition of physiological, psychological and social adaptability issued by the World Health Organization and according to the standards of “ compatibility with international scales and tools , conforms to the government's standards for the assessment of ...
Definition. Psychological assessment is a testing method that uses a number of techniques to find hypotheses about individuals and their behavior, abilities, and personality (Framingham 2016 ). Psychological testing or psychological assessment is also referred to as conducting a battery of psychological tests on subjects.
Health needs assessment is the systematic approach to ensuring that the health service uses its resources to improve the health of the population in the most efficient way. It involves epidemiological, qualitative, and comparative methods to describe health problems of a population; identify inequalities in health and access to services; and ...
Health administrative databases play a crucial role in population-level multimorbidity surveillance. Determining the appropriate retrospective or lookback period (LP) for observing prevalent and newly diagnosed diseases in administrative data presents challenge in estimating multimorbidity prevalence and predicting health outcome. The aim of this population-based study was to assess the impact ...
Health assessments can contribute important information that only a patient knows about his or her health and that might not be routinely acquired during typical office visits. In terms of prioritization, the provider reviews the problem list, then talks with the patient about possible treatment plans considering all of the different problems ...
A community health needs assessment (CHNA), sometimes called a community health assessment, is foundational for nonprofit healthcare organizations and a vital tool for hospitals and health systems working to improve population and public health. Completion of a CHNA every three years is a condition of maintaining 501 (r) (3) status as a ...
Background and Objective: High Lp(a) levels are a risk factor for ASCVD, however Lp(a) ordering in clinical practice is low. This study examines how race/ethnicity and socioeconomic status influence Lp(a) ordering. Methods: This is a single center, retrospective study (2/1/2020-6/30/2023) using electronic medical records of adults with at least one ICD-10 diagnosis of ASCVD or resistant ...
Exposure Assessment is the multi-disciplinary field that identifies and characterizes workplace exposures, develops estimates of exposure for exposure-response and risk assessment studies, and evaluates the significance of exposures and effectiveness of intervention strategies. Exposure assessment plays a central role in risk management.
Assessment of claimant, ... oncologists from subscriber institutions Lahey Hospital and Medical Center and Beth Israel Deaconess Medical Center to research and co-author this study that was published in the Journal of Healthcare Risk Management. ... "The Safety of Inpatient Health Care" study published in the New England Journal of Medicine on ...
Airborne pollutants pose a significant threat in the occupational workplace resulting in adverse health effects. Within the Industry 4.0 environment, new systems and technologies have been investigated for risk management and as health and safety smart tools. The use of predictive algorithms via artificial intelligence (AI) and machine learning (ML) tools, real-time data exchange via the ...

Crash of an Antonov AN-24 in Moscow

- Share the job
80m+ Private Motor Yacht
We are looking for a ETO for a 80m+ Private M/Y
The ideal candidate will be willing to help within the engineering team, whether that be helping the 2nd, being hands on or keeping the engine room clean.
Must have motor yacht experience 50m+ and some knowledge of AVIT.
Start: TBC Salary: €6500 per month Rotation: Time for time
This will be a shared cabin.
Work Experience Requirements:
Language requirements:.
Good knowledge of the English language is required.
Certificates and Qualifications:
A valid STCW Basic Safety Training certificate is required from all applicants. Please sign up for an STCW course and obtain the certificate if you don't have it yet.
Share this job:
Jobs on Yachts
- Deck Jobs (298)
- Engineering Jobs (99)
- Galley Jobs (139)
- Interior Jobs (282)
- Specialist Jobs (54)
- Shore Based Jobs (169)
- Other Jobs (24)
Email address:
Remember me Forgotten password?
Password Reset
Enter your email address and we will email you a password reset link.
Email address:

IMAGES
VIDEO
COMMENTS
Temporary ETO. 60m+ Private Motor YachtWe are looking for a temporary ETO for a 2 month temp gig on a 60m+ Joining last... 3 May 2024 - Undisclosed. Page 1 of 2. 1. 2. Next. View current job vacancies for a Eto on-board yachts, superyachts and megayachts.
Yacht Electronics Technical Officers (ETO) have 1+ years experience and are responsible for Day-to-day maintenance of all electronic, computer, audio/visual and communications equipment and ensures its efficient operation. They earn $48K-108K based on yacht size & experience. ... Job Responsibilities Day-to-day maintenance of all electronic ...
The ETOs take a specialist role within the Engineering Department and are responsible for maintaining a wide range of complex electric systems onboard a yacht. The responsibilities of an ETO include: Ensuring proper work and maintenance of all electrical equipment on board. Working of electrical parts like engine rooms, radio communications ...
Welcome to the Viking Crew maritime job search portal for ETO. The electro-technical officer is in charge of the ship's communications systems, electronic systems, and computer systems. As an ETO, you could work on a range of vessels from cargo ships and large vessels to passenger cruises and superyachts.
As for all crew working on board, to be a superyacht ETO you need to have completed your STCW basic safety training (a five day course) and have a valid ENG1 medical certificate. The ETO's remit was covered by a new Certificate of Competency (CoC) under regulation iii/6 of the STCW 2010 Manila Amendments. All crew sailing under the job title ...
ETO stands for Electro Technical Officer; many larger yachts have a full-time ETO. There is an official maritime certificate of competency as ETO, recognised by the International Maritime Organisation. On a merchant ship, this person would maintain the radios and the radars, the computer networks, and the navigation systems.
I asked experienced ETO Jameel 'Jimmy' Rahaman to share his story about how he got started, and to provide some pointers to those considering making the move. Name: Jameel Rahaman a.k.a. Jimmy. Age: 35. Nationality: Trinidadian. Qualification: CCNA, MCSE, MCSA, A+, N+, Security+, Studies in Information Sciences.
Being an ETO: The Good, the Bad and the Ugly. As an experienced superyacht ETO (Electro-Technical Officer), I wanted to share some insight into the role for anyone wanting to get into the superyacht industry. From fixing the captain's email account to troubleshooting an engine fault, the role of an ETO is extremely broad and the job can be very ...
May 3, 2024 - Mediterranean Approved. +4 more jobs. Log in or register to view 4 more Electronic Technical Officer (ETO) jobs. Page 2 of 2. Previous. 1. 2. View current job vacancies for a Eto on-board yachts, superyachts and megayachts.
The ETO works closely with the captain and other crew members to ensure that all systems are in proper working order and to troubleshoot and repair any issues that arise. They also may have a role in the maintenance and repair of the yacht's interior and exterior systems, such as air conditioning, lighting, and audio-visual equipment.
The role of ETO covers the yacht's audiovisual and communications systems, as well as maintaining all electrical and electronic equipment on board. From the yacht's radar and navigation systems to the WiFi, security systems and AV systems, the ETO's responsibilities are complex and ever-growing. The ETO works in the engineering department ...
USD ($)7,500.00 Per Month. Posted 5th May 2024. View Job. Electrical Technical Officer (ETO) This role is normally found on larger super yachts where there are a big team of engineers. They are responsible for all electrical equipment such as computers, GPS, navigational equipment to TVs, Internet and computers.
Yacht Engineer Job Roles. Chief Engineer. ... If going down the ETO route, there is a case for getting your ETO CoC III/6 as you will be working with HV and can be signed on as an ETO for manning requirements. Good electrical background or degree will also be highly advantageous. With AVIT there are a number of courses that would be useful ...
New job for ETO on Mega Yacht. An experienced ETO is required to join a 100M+ M/Y ASAP. Applicants must have prior experience in a similar role aboard yachts / passenger ships. The minimum certification needed would be: STCW, ENG1, ETO COC, DSD and High Voltage. On offer is a Euro salary and 182 days paid leave per year (3:3) Apply at: bit.ly ...
We offer yacht management services to a variety of exclusive superyachts. Our team excels in sourcing top-notch yacht crew positions, spanning from 25-meter private yachts in the Bahamas to 50-metre charter yachts in the Mediterranean to luxurious 100+ metre superyachts navigating the globe extensively. 81 yacht crew jobs available now.
Steve Jobs' wife, investor Laurene Powell Jobs, inherited a nearly finished yacht named Venus when the Apple co-founder died in 2011. After spending years holidaying on Ellison's yachts, Jobs ...
PRESQUE ISLE — Presque Isle Yacht Club, in association with Top O' Michigan Outboard Racing Club, presents the Fireside 500 Stock Outboard Race on Saturday and Sunday at The Fireside Inn ...
While not exactly a Sunfish, that boat is too small to count as a superyacht. At 106 meters, the Amadea, owned by a sanctioned Russian oligarch, definitely does. The $300 million yacht, which was ...
Gordon currently spends eight to 16 hours per day on her client's yacht, five to seven days per week. She posts to social media once each day, filming when she's not actively working. Her side ...
Zvenigorod's most famous sight is the Savvino-Storozhevsky Monastery, which was founded in 1398 by the monk Savva from the Troitse-Sergieva Lavra, at the invitation and with the support of Prince Yury Dmitrievich of Zvenigorod. Savva was later canonised as St Sabbas (Savva) of Storozhev. The monastery late flourished under the reign of Tsar ...
MQ2 Yacht Sold. MQ2 Sold. 'MQ2' is a 49.1m luxury yacht built and launched by Feadship. Delivered to a proud yacht owner in 1990 and refitted in 2015, 'MQ2' sleeps up to 14 guests in 6 staterooms and has accommodation for 10 crew members. MQ2 is a yacht sold by TWW, one of the leading brokerage houses with headquarters in Monaco.
The crew was engaged in a local training flight at Moscow-Sheremetyevo Airport consisting of takeoff and landings in strong cross winds. At takeoff, the right engine was voluntarily shut down.
March 17, 2011. Pavel Oderov was appointed as Head of the International Business Department pursuant to a Gazprom order. Pavel Oderov was born in June 1979 in the town of Elektrostal, Moscow Oblast. He graduated from Gubkin Russian State University of Oil and Gas with an Economics degree in 2000 and a Management degree in 2002.
80m+ Private Motor Yacht. We are looking for a ETO for a 80m+ Private M/Y. The ideal candidate will be willing to help within the engineering team, whether that be helping the 2nd, being hands on or keeping the engine room clean. Must have motor yacht experience 50m+ and some knowledge of AVIT. Start: TBC Salary: €6500 per month Rotation ...